Aging is a normal life process, which is subtle and is characterized by individual variation in onset and rate of decline. The basis of this process lies in changes in various macromolecules (from D.N.A. to membrane proteins) which primarily lead to alteration the form of function of a tissue or organ as a result of biological activity associated with a minor disturbance of normal cellular turnover.
In general the body experiences a decrease in blood microcirculation, cellular reproduction, tissue repair, metabolic rate, and an increase in development of excess fibrous connective tissue in an organ (fibrosis). With the degeneration of elastic and nervous tissues, these result in reduced function of most body systems.
How aging affects our mouth
Oral soft tissues
There is a decrease in the thickness of the epithelium, mucosa, and the submucosa is seen. Our taste bud function decreases. With age, an increase occurs in the number and size of Fordyce’s spots (sebaceous glands) on the cheeks, as well as lingual varices and foliate papillae on the tongue.
Nutritional deficiencies such as iron and vitamin B-12 are more prevalent in elders and these conditions may be associated with wasting of the oral mucosa and in particular with loss or reduction in the filliform papillae of the tongue.
Recent research suggests the stimulated salivary flow rate does not fall purely as result of age. However, medications of systemic disease can affect salivary output. This may lead to a diminished facility for chewing, poor retention of dentures, and digestive upsets. The dryness of mucosa renders it more susceptible to frictional irritation from dentures.
The toothless mucosa is frequently thin, lightly stretched and it blanches easily. Some of these characteristics may be found in elderly individuals. Their occurrence may well reflect the presence of systemic disease, nutritional disturbances or the side effects of medication. A variety of tissue overgrowth and ulcers have also been described in the elderly, mostly related to ill-fitting dentures.
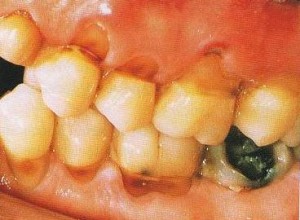
Dental hard tissues
Tooth enamel becomes less permeable with age and clinically older teeth appear more brittle. The rate of secondary dentine formation reduces with age, but still continues. Occlusion of the dentine tubules with calcified material spreads crown-wards with age.
Tooth wear is an age-related phenomenon and can be regarded as physiological in many cases. However, excessive and pathological wear can be caused by parafunction, abrasion, erosion (dietary, gastric or environmental) or a combination of these factors.
Dental pulp
There is increase fibrosis and decrease in blood supply to the pulp, which means that the defensive capacities of the pulp decrease with increasing age. Therefore pulp capping treatment is likely to succeed. Furthermore there is also an increase in secondary dentine and calcifications in the pulp.
Periodontium
There is an increase in fibrosis, decrease in number of cells, blood supply and cell turnover are found with increasing age. Whether gum recession is pathological or physiological is still hotly debated.
Systemic effects of aging in relation to dentistry
Immune system
A decrease in cell-mediated response and decrease in number of circulating lymphocytes leads to an increase incidence of autoimmune diseases as well as a decrease in the older patient’s defense against infection. Steroid treatment for autoimmune disease may complicate dental treatment
Nervous system
Aging involves both a physiological decline in function and dysfunction associated with age-related disease (for example strokes, Parkinson, trigeminal neuralgia). Aging may also impair the central processing of nerve impulses, impede the activity of striated muscles fibers and retard the ability to make decisions.
Cardiovascular system
Hypertension and ischemic heart disease worsens with age. Anemia is more common in the elderly. In general, then greater problems arise when a general anesthesia is required, or if the practice is on the second floor.
Degenerative arterial diseases can be considered as a universal accompaniment of aging in which is also seen in vessels of oral mucosa which make wounds heal more slowly and less effectively.
Pulmonary system
Lung capacity decreases with age and chronic obstructive airways disease increases in prevalence.
Endocrince system
Diabetes is more common as age increases.
Neuromuscular system
Muscle tone can decrease by as much as 20 to 25% in old age which explains the shorter chewing strokes and prolonged chewing time. There have been several reports of abnormal lower jaw movements consequent to the loss of natural teeth and increasing age.
Nutrition
Nutrition is one of the factors under human control that can influence the health of aging as the lack of essential nutrients can cause tissues friability and depress potential for repair.
Poverty, impaired mobility, decrease taste acuity and decrease chewing function can result in nutritional deficiencies n the elderly. These can manifest as changes in the oral mucosa.
Mucosal diseases which is more common with increasing age
- Oral cancer
- Lichen planus
- Herpes zoster is more common with increasing age due to decrease in T-cell function. Neuralgia occurs more frequently after an attack in the elderly
- Benign mucous membrane pemphigoid
- Pemphigus
- Candida or yeast infection is seen more frequently in the older age groups due to an increase proportion of denture wearers and increase immune deficiencies