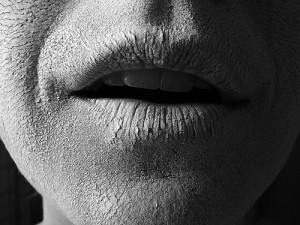
© Katie Tegtmeyer, Flickr.com
Saliva plays an important role in our daily lives. Saliva helps us swallow, talk, taste and protect our mouth and teeth. When there is a decrease in the amount of saliva in our mouth it can lead to dry mouth fatigue or also known as xerostomia.
Dry mouth can cause or increase risk of:
- tooth decay,
- gum diseases,
- bad breath,
- altered taste sensation,
- burning sensation of the tongue,
- sore mouth or cracks at the corners of the mouth,
- infections in the mouth
- difficulty in speaking and swallowing
- For people without teeth, denture retention, comfort and ability to chew and speak may become difficult when less saliva is present.
Sometimes you may complain of dry mouth but in fact, you have abundant of saliva. Having dry mouth at night, dry mouth in the morning or dry mouth while sleeping may occur as the saliva flow is naturally reduced at night or it can also be due to sleeping with your mouth open or breathing through your mouth. True or chronic dry mouth causes infection to the salivary glands, dry mouth and throat as well as tooth decay.
Dry mouth causes
Although the exact cause for dry mouth may be difficult to identify, the most common factors are the following:
- Sjogren’s syndrome
- Diabetes
- Emotional and anxiety states
- Menopause
- Negative fluid balance
- Selected nutritional and hormonal deficiencies
- Acquired immunodeficiency syndrome (AIDS)
- Anemia
- Frequent urination states
- Drugs or medications for example anti-hypertensives, anti-psychotics, anti-depressants, muscle relaxants, anti-histamines and laxatives
- Therapeutic radiation to the head and neck
- After bone marrow transplants
- Salivary gland disorders for example sialadenitis and salivary gland cancer
Dry mouth remedies
Treating dry mouth depends on the condition that is causing it. Generally, dry mouth treatment consists of managing the medical condition causing the dry mouth, increasing saliva flow and preventing tooth decay. The following are steps on how to manage dry mouth:

Dry mouth products © GlaxoSmithKline
- Use saliva substitutes to replace missing saliva and provide dry mouth relief.
- Frequent your water intake. Sip on juices and other fluids throughout the day. Take small sips of fluids with each bite of food at meal times.
- Stimulate saliva with sugar-free chewing gums, diabetic sweets or drugs and dry mouth products that stimulate salivation (as advised).
- Have frequent small meals. Avoid spicy, dry or hard crunchy foods. Take small bites and eat slowly. Moisten foods with gravies or sauce.
- Avoid anything that can worsen dry mouth, for example drugs, alcohol, smoking, caffeine and mouth-breathing.
- Prevent tooth decay by avoiding sugary foods or drinks.
- Prevent thrush and bad breath by keeping your mouth clean and as moist as possible. Remove dentures (if any) before you sleep and keep your dentures clean.
- Protect your lips using lip balm.
- Maintain a good oral hygiene by tooth-brushing and flossing twice a day and use a fluoridated toothpaste or dry mouth toothpaste like Orajel® and Biotene®. Use an alcohol-free mouthwash or a mouthwash for dry mouth.
- Have regular dental checkups to ensure your mouth stays healthy.
Dry mouth medications, such as cholinergic agents pilocarpine and bethanecol, may be prescribed by your doctor or dentist when your healthcare permits and if the dry mouth is severe.

© Cures For You
If you have true dry mouth your dentist would make frequent recalls to assess the tooth decay status. Aggressive tooth decay prevention efforts will be recommended because the presence of dry mouth puts you in a high-risk category for tooth decay. The following tooth decay-prevention efforts are essential to control tooth decay associated with dry mouth:
- Regular and thorough tooth brushing with both fluoride dentifrices and either high-dosage 2% sodium or 1.1% stannous home fluoride gel
- Removal of plaque between teeth through flossing and/or interproximal brushing
- Nutritional counseling
- Use of 0.12% chlorhexidine rinses
- Frequent professional removal of dead tissues (debridement)
- Frequent professional application of either 2% or 5% sodium fluoride
When to see a doctor or dentist

© McNEIL-PPC, Inc.
Do you have the following symptoms?
- Do you have reduced saliva flow?
- Do you sip liquids to help swallow dry foods?
- Does your mouth feel dry when you eat?
- Do you have difficulty swallowing what you eat?
- Do you feel the amount of saliva in your mouth seems to be too little?
- Do you have a sore or burning sensation in your mouth?
- Do you have difficulty in speaking for more than 10 minutes without drinking water?
- Do you need to suck on candies to assist the wetting of your mouth throughout the day?
If yes, please visit your attending doctor or dentist to confirm whether you are suffering from dry mouth or xerostomia.
Pingback: What is Sialadenitis? | Intelligent Dental
Pingback: How to Prevent Salivary Gland Cancer | Intelligent Dental
Pingback: Saliva Test Can Predict Tooth Decay and Drugs | Intelligent Dental
Pingback: Does Mouth Wash really work? | Intelligent Dental
Pingback: 10 Ways to Stop Bad Breath | Intelligent Dental
Pingback: How to Make Your Own Mouthwash Part1 | Intelligent Dental
Pingback: How Diabetes Can Affect Your Oral Health Part 2 | Intelligent Dental
Pingback: How to treat a Tooth with an Infected Old Crown | Intelligent Dental