Why White???
White colour is imparted due to any condition that increases the thickness of the epithelium thereby increasing the distance to the vascular bed.
Common causes are:
1. Hyperkeratosis
2. Acanthosis
3. Increased edema in the epithelium
4. Reduced vascularity in the lamina propria
White lesions and precancerous significance
International symposium held in Uppasala, Sweden 1994
Precancerous lesion: A morphologically altered tissue in which cancer is more likely to occur than in its apparently normal counterpart. Eg, oral leukoplakia
Precancerous condition: A generalized state associated with a significantly increased risk of cancer. Eg, Oral submucous fibrosis
Classification of white lesions of the oral mucosa
I HEREDITARY WHITE LESIONS
Leukoedema
White sponge nevus
Hereditary benign intraepithelial dyskeratosis
Dyskeratosis congenita
II REACTIVE / INFLAMMATORY WHITE LESIONS
Linea Alba
Frictional (traumatic) keratosis
Cheek chewing
Chemical injuries of the oral mucosa
Actinic Keratosis (Cheilitis)
Smokeless tobacco-induced keratosis
Nicotine stomatitis
Sanguinaria induced leukoplakia
III INFECTIOUS WHITE LESIONS, & WHITE & RED LESIONS
Oral hairy leukoplakia
Candidiasis
Mucous patches
Parulis
IV IDIOPATHIC “TRUE†LEUKOPLAKIA
V BOWEN’S DISEASE
VI ORAL LICHEN PLANUS
VII LICHENOID REACTIONS
VIII LUPUS ERYTHEMATOSUS (SYSTEMIC & DISCOID)
IX DEVELOPMENTAL WHITE LESIONS: ECTOPIC LYMPHOID TISSUE
X FORDYCE’S GRANULES
XI GINGIVAL AND PALATAL CYSTS OF THE NEWBORN AND ADULT
XII MISCELLANEOUS LESIONS
Geographic tongue
Hairy tongue (Black hairy tongue)
Oral submucous fibrosis
HEREDITARY WHITE LESIONS
LEUKOEDEMA
Common mucosal alteration
Variation of normal condition
Blacks (adults 90% and teenagers 50%)
White persons- variable (10 to 90%)
Similar edematous changes have been reported in other mucosal surfaces such as the vagina and larynx
Features :
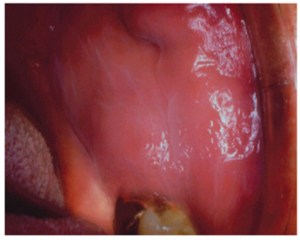
Site: Most frequently- buccal mucosa bilaterally
Rarely- labial mucosa, mucosa of the soft palate and floor of the mouth
Appearance: Faint, white, diffuse, and filmy, with numerous folds resulting in wrinkling of the mucosa
Non-scrapable
Disappears or fades upon stretching the mucosa
WHITE SPONGE NEVUS
Rare autosomal dominant disorder
High degree of penetrance and variable expressivity
Predominantly affects noncornified stratified squamous epithelium
Usually involves the oral mucosa, and less frequently the mucous membranes of the nose, esophagus, genitalia, and rectum
May be present at birth or may manifest or become more intense at puberty
Genetic analyses have identified a missense mutation in one allele of keratin 13 that leads to proline substitution for leucine within the keratin gene cluster on chromosome 17
Recent study using sequence analysis has reported a glutamine insertion localized in the helix initiation motif of the 1A alpha helical domain of Keratin 4 gene
Features :
Bilateral symmetric white, soft, “spongyâ€, or velvety thick plaques of the buccal mucosa
Other sites may be the ventral tongue, floor of the mouth, labial mucosa, soft palate and alveolar mucosa
Usually asymptomatic
No tendencies towards malignant change
Treatment :
No treatment is indicated for this benign and asymptomatic condition
If symptomatic, may require palliative treatment
One study has reported some relief of symptoms with a tetracycline rinse
HEREDITARY BENIGN INTRAEPITHELIAL DYSKERATOSIS
Also known as Witkop’s disease
Rare autosomal dominant disorder characterized by oral lesions and bilateral limbal conjunctival plaques
High degree of penetrance
Specifically seen in triracial isolate of white, Native American, and African American people and their descendants in Halifax county, North Carolina
Features:
Similar to WSN, with thick, corrugated, asymptomatic, white spongy plaques involving the buccal & labial mucosa
Other sites include floor of the mouth, lateral tongue, the gingiva, and palate
Generally detected in the 1st year of life and gradually increase in intensity until the teens
Involves bulbar conjunctiva where thick, gelatinous, foamy and opaque plaques form adjacent to the cornea
Ocular lesions usually manifest within the 1st year.
Few exhibit chronic relapsing ocular irritation & photophobia
Plaques may exhibit seasonal prominence with pronounced lesions in spring, & regression in summer
Few cases of blindness due to corneal vascularisation
Treatment:
No treatment required as it is a benign condition with regard to the oral lesions
For the ocular lesion, patient should be referred to an ophthalmologist
DYSKERATOSIS CONGENITA
Recessively inherited genodermatosis
Rare X-linked disorder characterised by a series of oral changes that eventually lead to an atrophic leukoplakic oral mucosa, with the tongue and cheek most severely affected
High incidence of oral cancer in affected adults
Oral changes occur in association with severely dystrophic nails and a prominent reticulated hyperpigmentation of the skin of the face, neck & schest
Many cases exhibit hematologic changes including pancytopenia, hypersplenism and an aplastic or Fanconi’s anemia
Oral lesions commence before the age of 10 yrs as crops of vesicles with associated patches of white ulcerated necrotic mucosa often infected with Candida
Erythroplakic changes and nail dystrophy follow, with leukoplakic lesions and carcinoma supervening on the oral lesions in early adulthood