Saliva is essential to oral health and individuals who have too much or too little saliva can affect many functions, and may develop infections as a consequence of the reduced defenses.
Saliva has many functions. Saliva helps us swallow, talk, taste and protect our mouth and teeth. Saliva not only physically removes dietary substrates and acids produced by plaque from the mouth, but it has a most important role in buffering the pH in saliva and within plaque. Fast-flowing saliva is alkaline and is vitally important in raising the pH of tooth plaque previously lowered by exposure to sugar and carbohydrates. Low pH can lead to demineralization of tooth substance which can initiate tooth decay. Saliva can also be used to detect drugs in our body system and it may also help in diagnosing certain diseases therefore do not underestimate this watery substance in your mouth.
Having too much saliva
Drooling is defined as saliva beyond the margins of lips. The condition of increased salivary flow is termed sialorrhoea or ptyalism. This condition occurs in people at the extremes of age, the chronically debilitated or those in chronic care facilities, especially associated with stroke and esophageal cancer, are especially affected. Drooling is perfectly normal in healthy infants but usually stops by about 18 months of age and is considered abnormal if persists beyond the age of 4 years. However sleep drooling is normal especially if the person is a mouth-breather.
Drooling causes
Drooling is caused either by increased salivary flow (sialorrhoea) that cannot be compensated for by swallowing or by poor oral and facial muscle control in individuals with swallowing dysfunction (secondary sialorrhoea) or by anatomic or neuromuscular anomalies.
- Excessive saliva production (sialorrhoea) – neurologic disorders (especially Riley-Day syndrome), otolaryngologic (ear, nose and throat) diseases, pregnancy, gastrointestinal causes, liver disease, oral lesions, cholinergic drugs, anti-cholinesterases
- Decreased swallowing – oropharyngeal (relating to or located near the cavity formed by the pharynx at the back of the mouth) infections and obstruction
- Anatomic abnormalities – macroglossia (large tongue) or tongue thrusting, surgical defects following major head and neck resection
- Neuromuscular diseases – Parkinson’s disease, cerebral palsy, intellectual disability, stroke, pseudobulbar palsy or bulbar palsy
Clinical features of drooling
Mouth drooling impacts on affected individuals, families and caregivers:
- Functionally – saliva soils the clothing of the person, peers, siblings, parents and caregivers as well as furniture. Clothing and bibs become soiled and need frequent changing.
- Socially – embarrassment may make it difficult for individuals to interact with their peers and can lead to isolation
- Psychologically – stigmatism is common
- Clinically – unable to manage their oral secretions, affected persons are at increased risk of skin maceration (Softening due to soaking), infection and aspiration. Affected individuals may experience repeated skin breakdown and infections around the mouth. Aspiration-related respiratory and pulmonary complications are greatest in those with a diminished sensation of salivary flow and hypopharygeal retention. In rare severe cases, dehydration may become a problem.
Quantitation of drooling
- Dry – never drools
- Mild – only lips wet. Occasional drooling – not every day
- Moderate frequent drooling – lips and chin wet – every day
- Constant drooling: severe – clothing soiled, profuse – hands moist and wet
Management of drooling
The impact of drooling on the quality of life is the most important factor in determining the need for treatment. The goal is to reduce drooling whilst maintaining a moist, healthy oral cavity. Treatment is best done by a team approach, including at least an otolaryngologist, neurologist, surgeon, dentist, orthodontist, speech, occupational and physical therapists. Treatment options include medical therapy, radiotherapy and surgery.
Medical therapy
- Oral motor training exercises can be used to try to normalize muscle tone, increase lip closure and promote swallowing.
- Behavior training, biofeedback and automatic cueing techniques
- Pharmacotherapeutics attempts to decrease saliva to amounts that can be swallowed (to prevent ‘pool and drool’) without producing dry mouth by:
- Reducing cholinergic activity, either systematically (for example atropine-related oral anti-cholinergics) or more locally (for example sublingual ipratropium spray). Because of potential adverse effects, anti-cholinergic drugs are contraindicated in individuals with asthma, or ocular problems, such as glaucoma.
- Increasing adrenergic activity (for example clonidine or scopolamine patch)
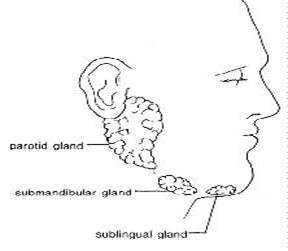
- Botulinum toxin type A injected under ultrasound guidance into the parotid and submandibular glands.
Radiotherapy
Irradiation of the major salivary glands has been used to decrease saliva secretion but has variable success and the potential risk of cancer later in life.
Surgery
Surgery is indicated where there is drooling:
- Persisting after at least 6 months of conservative therapy OR
- Moderate to profuse or excessive drooling and in a patient whose cognitive function prevents use of conservative therapy.
Surgical procedures used to control drooling are aimed at decreasing salivary flow or redirecting the salivary direct flow o a location more advantageous to promote swallowing and include salivary gland excision, duct re-routing, duct ligation, nerve sectioning, or combination of the above.
To be continued in Part 2