Bacteria in dental plaque are the direct cause of the most widespread of all human diseases – dental cavities and inflammatory gum or periodontal diseases. These diseases, however, are not classical infections. They arise because of complex changes in plaque ecology and are affected by many factors in the host’s protective responses.
How does dental plaque form?
To understand the role of dental plaque in disease and how to prevent or control the plaque-associated dental diseases, it is essential to understand the nature of dental plaque. Teeth plaque forms initially on the organic layer coating the erupted tooth. This organic layer originates from salivary products that are deposited on the teeth, forming an acquired pellicle to which bacteria adhere. Dental caries or cavities-related bacterial species have a greater ability than others to adapt to excess sugars and their metabolites.
How does plaque affect the teeth
Dental plaque is composed of salivary proteins that adhere to the teeth, plus bacteria and end-products of bacterial metabolism. Both decay-causing and gum disease-causing organisms accumulate in the plaque located along the gum margin, in between teeth, and in the pits and fissures. Tooth plaque collects more profusely in these specific areas because none of these locations is optimally exposed to the normal self-cleansing action of the saliva, the abrasive action of foods, or the muscular action of the cheeks and tongue. Plaque decreases in thickness as the chewing or tip of the tooth surface is approached. Little plaque is found on the chewing surface except in the pits and fissures. As would be expected, plaque forms more profusely on crooked teeth or on teeth with orthodontic appliances, where access for cleaning is often difficult.
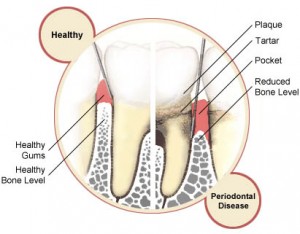
It is important to differentiate between the supragingival and the subgingival plaques. The supragingival plaque can be seen above the gum margin on all tooth surfaces; the subgingival plaque is found in the sulcus and pocket below the gum margin, where it is not visible. Supragingival plaque on teeth is associated with cavities and gingivitis, whereas subgingival plaque is associated with gingivitis and periodontitis. The disease-causing capacity of each of the plaques can vary independently of the other. For example, it is possible to have periodontal disease with or without tooth decay, to have neither, or to have a shifting status of cavities or periodontal disease, or both.
The disease-causing capacity or pathogenicity of the subgingival plaque is becoming an increasing concern. Not only does it cause periodontal disease, which is a lifelong debilitating disease of the tooth supporting tissues, but it is now believed that there is a causal relationship between periodontitis and such diverse conditions as, cardiovascular disease, diabetes mellitus, chronic respiratory disease, and immune function. There is also the possibility in some cases that this is a bi-directional association where the oral problem begins with a systemic condition, instead of vice versa.
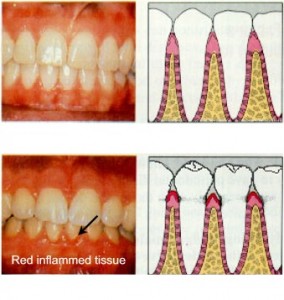
Not only does the daily dental plaque removal reduce the probability of dental cavities; equally important, it also reduces the possibility of the onset of inflammation of the gums or gingivitis. This occurs when the metabolic end-products of the organisms that are contained in the plaque irritate the adjacent gum tissues, producing an inflammation (for example gingivitis). If the inflammation continues, bleeding (hemorrhage) can be expected following even minimal pressure (“pink toothbrush”). This gingivitis can be arrested and reversed (cured) in the early stages by proper brushing, flossing, and irrigation, especially if accompanied with professional guidance.
Plaque concentrates mineralizing ions such as calcium, phosphate, magnesium, fluoride and carbonates from the saliva to provide the chemical environment for the precipitation and formation of calculus or dental tartar, a concretion that adheres firmly to the teeth. If the plaque removal is not done by flossing and brushing before the calculus begins to form, the resultant mineralized mass provides a greater surface area for an even more damaging plaque accumulation. This additional mass of plaque organisms covering the rough porous surface causes the stagnation of even more bacteria and is responsible for the damage to the periodontal or tooth supporting tissues. Also, the hard, irregular calculus deposits pressing against the soft tissues serve to worsen the inflammation caused by the bacteria alone.
How to remove dental plaque
Regular toothbrushing and flossing can remove dental plaque and control its formation. Once dental plaque mineralizes to form calculus, professional instrumentation such as dental scaling is necessary for its removal. Notwithstanding the contribution of calculus to inflammatory periodontal diseases, it is stagnation of disease-causing bacteria at critical sites that leads to both dental cavities and periodontal diseases.
To this point, only mechanical plaque control (for example the use of a toothbrush, dental floss, and an irrigator) has been highlighted. Rapidly growing in importance as a supplement to mechanical plaque control (but not as a replacement), is chemical plaque control. This approach utilizes mouthrinses containing antimicrobial agents that effectively help control the plaque bacteria involved in causing both cavities and gingivitis. For helping to control gingivitis, a popular and economical over-the-counter product is Listerine and the most effective prescription rinse is chlorhexidine.