 What is gingivitis?
What is gingivitis?
Gingivitis or generally known as gums (gingiva) disease is defined as an inflammation of the gums surrounding the teeth. Gingivitis is commonly initiated by dental plaque formation, termed as plaque-induced gingival disease. With continuous plaque irritation and severe inflammation to the gums, this condition will progress into periodontitis, a destructive form of periodontal disease.
However, non-plaque-induced gingival lesion is an oral manifestation of systemic conditions that produce lesions in the gums; which are in very rare occurrence.
Do I have gum disease?
If you notice your gums become:
- redness, swollen and shiny
- soft or spongy texture and ulcerated
- gums that are tender to touch
- spontaneous bleeding occurs while brushing or even flossing
- sometimes it may also produce a foul odor
Comparatively, a healthy gum will appear coral-pinkish, firm in texture, knife-edged well-contoured stippling and do not bleed easily.
How does gum disease occur?
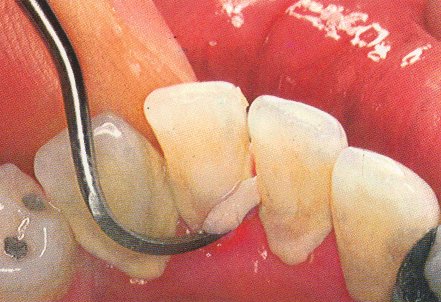
Dental plaque formation is a natural, physiological process. Clinically, it is seen as a structured, resilient, yellow-grayish substance that adheres tenaciously to the tooth surfaces. Plaque is a bacteria biofilm which is a complex association of many different bacterial species living together in a single environment in our mouth. It is not a haphazard collection of bacteria but it is a community of microorganisms coexists at a state of balance.
However, when disruption of this balance occurs, it may cause alterations in your mouth and resulting in destruction of gum tissues.
Gingivitis is very common and ranging from mild to severe inflammation. Sometimes it can be very mild that you are not aware of having the condition as well.
 What are the risk factors to gingivitis?
What are the risk factors to gingivitis?
a)Â Â Â Â Poor oral hygiene
b)Â Â Â Â Tobacco smoking
c)Â Â Â Â Predisposing (plaque-retentive) factors
Poor technique when restoring teeth can result overhanging fillings such as amalgam fillings; which occur frequently at interproximal sites of teeth. Overhangs render interproximal cleaning and hence, result in plaque-induced inflammation.
Others include: badly-designed dentures, wearing orthodontic appliances, tooth malalignment, food impactions in between teeth, defective crown/bridges margin and lack of lip-seal or mouth-breathing.
d)Â Â Â Â Hormonal changes
For certain individual cases, effects of gingivitis are exaggerated during puberty, menstruation, taking oral contraceptives and during pregnancy (starting at third month from gestation and peak at six months, complete resolution only at parturition).
e)Â Â Â Â Systemic disease such as Diabetes Mellitus
Severe uncontrolled Diabetes Mellitus increased risk of developing gingivitis. However, well-controlled diabetics will minimize the growth of disease.
f)Â Â Â Â Â Â Drugs interaction
Some degree of gums inflammation is seen in epileptic drugs (phenytoin/epanutin), immunocompressive drugs (cyclosporin) and calcium channel blocking drugs to treat cardiac arrest, angina and hypertension (nifidepine).
g)Â Â Â Â Decreased immunity such as leukemias and HIV/AIDS related diseases
h)Â Â Â Â Genetic factors
i)Â Â Â Â Â Â Â Old age
j)Â Â Â Â Â Â Â Poor nutrition and low socioeconomic status
 How do we treat gum disease?
How do we treat gum disease?
Our main focus of treatment is to remove the causative agent i.e. dental plaque.
- The best way is to give proper Instruction for home care
- It is very important to maintain a good dental hygiene with proper tooth brushing with fluoridated toothpaste. Seek for advices from your dentist on the effective techniques of tooth brushing. Flossing and usage of antiseptic mouthwashes are recommended to clear the mouth from food debris and reduce the activity of odor-producing microorganisms.
- Plaque cannot be removed by rinsing or the use of sprays. Proper professional dental cleanings like scaling and curettage are recommended. Depending on the severity of gingivitis, your dentist may opt for gum surgery.
- Correction of predisposing (plaque-retentive) factors, misaligned teeth or bad restorations.
- If any of these contributing to your gum disease, your dentist will recommend fixing these problems as well.
What is the most simple step that can be taken to prevent gum disease
The best way to prevent gingivitis is from a good dental hygiene practice consistently throughout life.
- Brush twice a day, every morning and before bed at night.
- A thorough cleaning with a toothbrush should take one to two minutes.
- Flossing before you brush allows you to clean away the loosened food particles and bacteria.
- Do regular check-ups to your dentist every 6 months once for a good oral care.
- If you have risk factors that increase your chance of developing gingivitis, you may need professional dental cleanings more often.
- Use a soft-bristle toothbrush and proper size toothbrush head according to your mouth size.
- Replace your toothbrush every three to four months.
- Consider using an electric toothbrush which may be more effective at removing plaque.
- Floss daily or use interdental brushes to clean between your teeth.
- Use mouthwashes to help reduce plaque on your teeth.