What is Root Canal Treatment (RCT)?
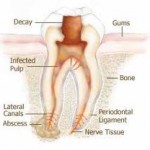 Root canal treatment is the removal of inflamed and/or infected dental pulp tissue from the root canal system, shaping and filling the root canals of a diseased tooth. The key factor in the development of pulpal inflammation and breakdown of the supporting tissues of the tooth (periradicular tissues) is the presence of bacteria. These endodontal infections (infections within teeth) are usually characterized by loss of integrity of the crown, invasion by bacteria, and destruction of enamel, dentine, and eventual pulpal involvement. Dental caries, trauma, tooth surface loss, and microleakage around tooth fillings can lead to endodontal infection. In situations where there has been periradicular breakdown, root canal treatment will result in the return of the health of the periradicular tissues. Ultimately, root canal treatment preserves teeth as functional units within the dental arch.
Root canal treatment is the removal of inflamed and/or infected dental pulp tissue from the root canal system, shaping and filling the root canals of a diseased tooth. The key factor in the development of pulpal inflammation and breakdown of the supporting tissues of the tooth (periradicular tissues) is the presence of bacteria. These endodontal infections (infections within teeth) are usually characterized by loss of integrity of the crown, invasion by bacteria, and destruction of enamel, dentine, and eventual pulpal involvement. Dental caries, trauma, tooth surface loss, and microleakage around tooth fillings can lead to endodontal infection. In situations where there has been periradicular breakdown, root canal treatment will result in the return of the health of the periradicular tissues. Ultimately, root canal treatment preserves teeth as functional units within the dental arch.
RCT is carried out in 2 phases:
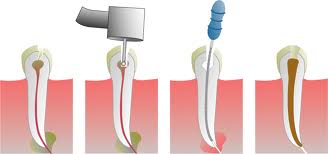
1.     Root canal preparation
- Involves the removal of organic material, including inflamed/infected pulp tissue, bacteria that may have invaded the root canal system and infected dentine from the root canal system, and
- shaping of the root canal system to facilitate placement of a root canal filling material
2.     Root canal filling
Current tooth preparation techniques do not eliminate bacteria completely, therefore root canal filling is necessary to:
- entomb any remaining bacteria within the root canal system
- prevent re-infection by denying new bacteria (from the mouth) entrance into the tooth
- prevent entry of periradicular tissue fluid which may be a continuing nutritional supply for the remaining bacteria inhabiting the root canal system
Following root canal filling, an adequate and timely tooth restoration is given to restore the integrity of the tooth.
When do you need a RCT?
RCT is generally indicated in situations where the endodontal diseases have progressed and are affecting the dental pulp and periradicular tissues. The conditions which might require RCT and their possible associated signs and symptoms include:
1.     Pulpal conditions
-
irreversible inflammation of the pulp (irreversible pulpitis)
-Â Â usually presents as a dull, throbbing tooth pain that lingers for minutes up to several hours; it may be spontaneous or initiated by temperature changes (for example, hot/cold drink).
-Â Â The pain may be worse at night or when you bend or lie down; this is due to an increase in pressure within the pulp brought about by these postural changes.
-Â Â When periradicular inflammation is also present, the tooth may be tender to touch.
-Â Â The affected tooth may be difficult to localize and its radiograph tends to be within normal limits; radiographic changes are only recognized when the inflammation extends to the periradicular tissues.
-Â Â The pulp is referred to as being irreversibly inflamed because the removal of the causal factor does not lead to recovery to a healthy state; if untreated, the pulp will eventually become dead (necrotic).
-Â Â The treatment options: RCT or extraction

-
Hyperplastic pulpitis
-  refers to the proliferation of pulp tissue to produce a ‘pulp polyp’ resulting from irritation usually associated with large caries exposure in young patients.
-Â Â usually symptomless with no radiographic changes.
-Â Â Treatment options: RCT or extraction.
-
Pulp necrosis
-Â Â describes partial or total death of pulp tissue as a result of loss of adequate blood supply
-  The tissue may not yet be infected, particularly if it was caused by trauma that led to the compromise of the tooth’s blood supply.
-Â Â The tooth will not normally respond to electrical and thermal pulp vitality tests and no radiographic changes will be seen.
-Â Â This will eventually result in the development of periradicular periodontitis. (see periradicular conditions below)
-Â Â Treatment options: RCT or extraction.
-
Pulp calcification
-Â Â describes partial or total obliteration of the pulp space due to deposition of tertiary dentine in response to an irritant.
-Â Â The crown of the tooth may look darker in color compared to the neighboring teeth (due to tertiary dentine deposition in the pulp chamber).
-Â Â usually painless, unless accompanied by necrosis and bacterial infection.
-Â Â Vitality testing is not always likely to produce a response.
-Â Â RCT is indicated only if symptoms indicate irreversible pulpitis or there are radiographic changes showing periradicular breakdown.
2.     Periradicular conditions due to the presence of infected pulp
-
Periradicular periodontitis
-Â Â Â Â Â Â Â Â refers to inflammatory changes within the periodontal ligament.
-Â Â Â Â Â Â Â Â can be due to pulp infection spreading into periodontal ligament or to occlusal trauma.
-Â Â Â Â Â Â Â Â You will feel tenderness on biting and clinical examination will reveal tenderness to percussion.
 -Â Â Â Â Â Â Â Â Tooth may not respond to pulp vitality testing indicating pulp necrosis; in addition, there may be a sinus tract found in the mouth or outside on the skin with the presence of a gumboil, bad taste or smell; RCT or extraction is thus indicated
-Â Â Â Â Â Â Â Â Tooth may not respond to pulp vitality testing indicating pulp necrosis; in addition, there may be a sinus tract found in the mouth or outside on the skin with the presence of a gumboil, bad taste or smell; RCT or extraction is thus indicated
-Â Â Â Â Â Â Â Â If symptoms are due to occlusal trauma, examination may reveal a high spot on a recent filling and/or a positive response to vitality testing (indicating a living tooth); occlusal adjustments are necessary.
-
Periradicular abscess
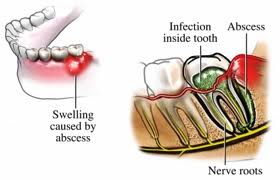 -Â Â Â Â Â Â Â Â is a localized collection of pus which usually occurs in the gum area associated with an infected tooth
-Â Â Â Â Â Â Â Â is a localized collection of pus which usually occurs in the gum area associated with an infected tooth
-Â Â Â Â Â Â Â Â The symptoms range from mild to severe pain and swelling with tenderness to touch and mobility of the tooth.
-Â Â Â Â Â Â Â Â There may be accompanying vague feeling of discomfort (malaise), fever and lymph node enlargement.
-Â Â Â Â Â Â Â Â Drainage of pus is necessary and antibiotics may be required; once the swelling resolves, RCT or extraction may be carried out.
Once a diagnosis has confirmed any of the above conditions, an assessment of the marginal periodontal status and restorability of the tooth is necessary to determine whether RCT or extraction is to be done. RCT can be carried out if there is satisfactory periodontal health and the tooth is restorable. If not, the tooth needs to be extracted.
please send me reqular uddates on dental health
Thanks for your interest. Please subscribe to our RSS feed for regular updates. If you like us. please fan (like) our Facebook page.
how long does a route canal take to heal after
During RCT, the inflamed and/or infected dental pulp tissue from the root canal system is removed and medicaments will be placed within the root canal between appointments as long as symptoms are still present to further reduce the infection. Only after the symptoms are all resolved, the dentist will carry out root canal filling. By this time, the root canal system is considered bacterial free and the root canal filling is served to prevent re-infection. For teeth with periradicular conditions, the periodontal status will heal thereafter depending on individual variation.
I have consistent pain in the last tooth right,it’s not loose but maybe must be extracted