Temporomandibular disorders (TMD) is the term for non-specific diagnosis that represents a group of often painful and/or dysfunctional conditions involving the muscles of mastication or the temporomandibular joint (TMJ) or both.
What is TMJ?
Temporomandibular joint is the joint of the jaw and there are two TMJs, one on each side of the face. The name is derived from the two bones which form the joint: the upper temporal bone which is part of the cranium (skull), and the lower jaw bone called the mandible.
Classification of temporomadibular disorders
- Masticatory muscle disorders
- Disc interference disorders
- Inflammatory arthritis -Traumatic arthritis, Degenerative arthritis (osteoarthritis), Rheumatoid arthritis
- Ankylosis -Fibrous,Bony
- Growth disorders
- Aberrant development – Condylar hyperplasia, condylar hypoplasia
- Tumors
- Bone (osteoma)
- Cartilage (osteochondroma)
Most common temporomandibular disorders, comprising 90 to 95% of all temporomandibular disorders cases, is a condition with multiple musculoskeletal facial pain complaints and a variety of jaw dysfunctions and without an identifiable structural cause. The diagnosis will most likely be myofascial pain, internal derangement or osteoarthrosis.
What is myofascial pain?
Myofascial pain, a chronic pain disorder due to central nervous system-induced involuntary contraction of masticatory muscles, is categorized under masticatory muscle disorders. This condition was previously named temporomandibular pain dysfunction syndrome, myofascial pain dysfunction syndrome and masticatory myospasm.
This is the commonest cause of complaint involving the temporomandibular joint and it has three cardinal symptoms: pain associated with the joint or its musculature, clicking of the joint and limitation of jaw movement.
There is continuous muscle contraction affecting the elevator muscles resulting in pain on opening and chewing and trismus (limited mouth opening), as well as the lateral pterygoid which causes pain on clenching, protrusion and lateral excursion and acute malocclusion. It is a self-perpetuating myospasm cycle. Myofascial pain may occur alone, be secondary to internal derangement or play a major role in causing internal derangement.
Who is more likely to have myofascial pain?
More commonly seen in women than in men between age 15 and 40 years, myofascial pain is associated with history of stress, anxiety or depression. It may even be a manifestation of chronic pain with a behavioral disorder. Diagnostic information is based on the symptom picture, past dental history and social history.
Myofascial pain symptoms and signs
Myofascial pain can also produce a variety of other symptoms, which may includes:
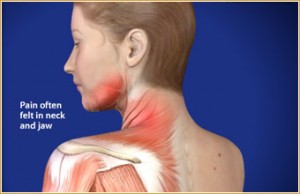
- Diffuse pain over one side of the face which could be mild or severe especially around the muscles of mastication
- The pain fluctuates in intensity and may be exacerbated for several hours or days
- Pain is worse in early mornings or early evenings
- Knots in the muscles (trigger points)
- Disturbed sleep
- Jaw movements are painful
- Clicking or crepitus (crunching sound) of the joint
- There may be restricted opening of the mouth with or without locking of the TMJ
- Unilateral tooth loss or other dental irregularities are very common, but there is no consistent relationship between the side of occlusal disharmony and the side of joint symptoms.
- There is a strong clinical impression that the condition has a relationship with various types of emotional stress. Bruxism is common and many sufferers have nocturnal tooth-grinding habits.
Investigations
- X-rays or radiographs including orthopantomogram radiograph is done to exclude any bone disease in the TMJ. No structural changes are usually seen in myofascial pain.
- Referral for behavioral or psychological assessment if required
Management of myofascial pain
Principles of management are based on an accurate diagnosis and each individual’s needs, which should be non-invasive, conservative and reversible.
Aims of treatment are to control pain, limit function, and relax muscles. Combination of treatment modalities is often successful.
Myofascial pain treatment methods
- Explanation or counseling for reassurance that the condition is benign and frequently self-limiting to avoid anxiety over the condition
- Conservative advice is given to rest the muscles. Soft diet, limit mouth opening or chewing on both sides are usually advised
- Application of heat to reduce spasm. Moist heat or balm is applied over the painful muscle
- Muscle relaxant tables to reduce spasm.
- Muscle exercises to re-educate muscles. Exercises are for correcting abnormal joint movements and ‘hinge opening’
- Correct occlucal problems by providing balanced function, replacing missing teeth and correcting occlusal faults
- Splint therapy to reduce muscle activity. Occlusal splints, for example stabilization splint, can be prescribed
- Physiotherapy to increase muscle blood flow such as short wave diathermy and ultrasound
- Psychotherapy to change perception of pain so that there is self-management or self control over pain