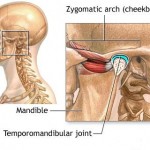
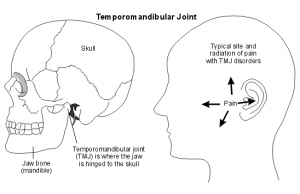
Temporomandibular joint disorder (TMJD or TMD), or TMJ syndrome, is an umbrella term covering acute or chronic inflammation of the temporomandibular joint, which connects the mandible to the skull. The disorder and resultant dysfunction can result in significant pain and impairment. Because the disorder transcends the boundaries between several health-care disciplines—in particular, dentistry and neurology—there are a variety of treatment approaches.
 The temporomandibular joint is susceptible to many of the conditions that affect other joints in the body, including ankylosis, arthritis, trauma, dislocations, developmental anomalies, neoplasia and reactive lesions.
The temporomandibular joint is susceptible to many of the conditions that affect other joints in the body, including ankylosis, arthritis, trauma, dislocations, developmental anomalies, neoplasia and reactive lesions.
An older name for the condition is “Costen’s syndrome”, after James B. Costen, who partially characterized it in 1934.
Signs and symptoms of temporomandibular joint disorder vary in their presentation and can be very complex, but are often simple. On average the symptoms will involve more than one of the numerous TMJ components: muscles, nerves, tendons, ligaments, bones, connective tissue, and the teeth. Ear pain associated with the swelling of proximal tissue is a symptom of temporomandibular joint disorder.
Symptoms associated with TMJ disorders may be:
- Biting or chewing difficulty or discomfort
- Clicking, popping, or grating sound when opening or closing the mouth
- Dull, aching pain in the face
- Earache (particularly in the morning)
- Headache (particularly in the morning)
- Hearing loss
- Migraine (particularly in the morning)
- Jaw pain or tenderness of the jaw
- Reduced ability to open or close the mouth
- Tinnitus
- Neck and shoulder pain
- Dizziness
Temporomandibular joints
 Unlike a typical finger or vertebral junctions, each TMJ actually has two joints, which allows it to rotate and to translate (slide). With use, it is common to see wear of both the bone and cartilage components of the joint. Clicking is common, as are popping and deviations in the movements of the joint. Pain is the most conventional signifier of TMD.
Unlike a typical finger or vertebral junctions, each TMJ actually has two joints, which allows it to rotate and to translate (slide). With use, it is common to see wear of both the bone and cartilage components of the joint. Clicking is common, as are popping and deviations in the movements of the joint. Pain is the most conventional signifier of TMD.
The surfaces in contact with one another (bone and cartilage) do not have any receptors to transmit the feeling of pain. The pain therefore originates from one of the surrounding soft tissues, or from the trigeminal nerve itself, which runs through the joint area. When receptors from one of these areas are triggered, the pain can cause a reflex to limit the mandible’s movement. Furthermore, inflammation of the joints or damage to the trigeminal nerve can cause constant pain, even without movement of the jaw.
Due to the proximity of the ear to the temporomandibular joint, TMJ pain can often be confused with ear pain. The pain may be referred in around half of all patients and experienced as otalgia (earache). Conversely, TMD is an important possible cause of secondary otalgia. Treatment of TMD may then significantly reduce symptoms of otalgia and tinnitus, as well as atypical facial pain. Despite some of these findings, some researchers question whether TMD therapy can reduce symptoms in the ear, and there is currently an ongoing debate to settle the controversy.
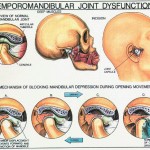
The dysfunction involved is most often in regards to the relationship between the condyle of the mandible and the disc. The sounds produced by this dysfunction are usually described as a “click” or a “pop” when a single sound is heard and as
“crepitation” or “crepitus” when there are multiple, rough sounds.
Teeth
 Disorders of the teeth can contribute to TMJ dysfunction. Impaired tooth mobility and tooth loss can be caused by destruction of the supporting bone and by heavy forces being placed on teeth. The movement of the teeth affects how they contact one another when the mouth closes, and the overall relationship between the teeth, muscles, and joints can be altered. Pulpitis, inflammation of the dental pulp, is another symptom that may result from excessive surface erosion. Perhaps the most important factor is the way the teeth meet together: the equilibration of forces of mastication and therefore the displacements of the condyle. Many report TMJ dysfunction after having their wisdom teeth extracted.
Disorders of the teeth can contribute to TMJ dysfunction. Impaired tooth mobility and tooth loss can be caused by destruction of the supporting bone and by heavy forces being placed on teeth. The movement of the teeth affects how they contact one another when the mouth closes, and the overall relationship between the teeth, muscles, and joints can be altered. Pulpitis, inflammation of the dental pulp, is another symptom that may result from excessive surface erosion. Perhaps the most important factor is the way the teeth meet together: the equilibration of forces of mastication and therefore the displacements of the condyle. Many report TMJ dysfunction after having their wisdom teeth extracted.
Cause
There are many external factors that place undue strain on the TMJ. These include but are not limited to the following:
Bruxism has been shown to be a contributory factor in the majority of TMD cases. Over-opening the jaw beyond its range for the individual or unusually aggressive or repetitive sliding of the jaw sideways (laterally) or forward (protrusive). These movements may also be due to parafunctional habits or a malalignment of the jaw or dentition. This may be due to:
- Bruxism (repetitive unconscious clenching or grinding of teeth, often at night).
- Trauma
- Malalignment of the occlusal surfaces of the teeth due to defective crowns or other restorative procedures.
- Jaw thrusting (causing unusual speech and chewing habits).
- Excessive gum chewing or nail biting.
- Size of food bites eaten.
- Degenerative joint disease, such as osteoarthritis or organic degeneration of the articular surfaces, recurrent fibrous and/or bony ankylosis, developmental abnormality, or pathologic lesions within the TMJ
- Myofascial pain syndrome
- Lack of overbite
 Patients with TMD often experience pain such as migraines or headaches, and consider this pain TMJ-related. There is some evidence that some people who use a biofeedback headband to reduce nighttime clenching experience a reduction in TMD. The
Patients with TMD often experience pain such as migraines or headaches, and consider this pain TMJ-related. There is some evidence that some people who use a biofeedback headband to reduce nighttime clenching experience a reduction in TMD. The
dentist must ensure a correct diagnosis does not mistake trigeminal neuralgia as a temporomandibular disorder.