Your dentist referred you to an endodontist for a root canal treatment that he/she finds difficult to do. However you started having the jitters about your endodontic appointment since this is a specialist you are seeking. This article will give you a gist on what happens at an appointment with an endodontist.
What is an endodontist?
An endodontist is a professional who practices a specialty field of dentistry is known as endodontology. Endodontology or Endodontics (from the Greek endo “inside”; and odont “tooth”) is the specialty of dentistry that studies the tooth pulp and the tissues surrounding the root of a tooth, and the diseases as well as conditions that affect them.
What does an endodontist treat?
Root canal therapy is one of the most common procedures performed by an endodontist. However they also perform a variety of procedures including retreatment of failed root canal therapy, endodontic surgery, as well as treating cracked teeth and dental trauma. Because they limit their practices to endodontics, endodontists use their special training and experience in treating difficult cases, such as teeth with narrow or blocked canals, or unusual anatomy.
Endodontists may use advanced technology, such as operating microscopes, ultrasonics and digital imaging, to perform these special services.
Who should see an endodontist?
A general dentist can manage some simple root canal needs but more complex cases that require root canal therapy in teeth with multiple root configuration or surgical procedures would need to be handled by a root canal specialist.
A dentist will usually refer certain cases to an endodontist that include:
- Complex root canal treatment procedures.
- Abscessed tooth that require surgical procedures.
- When complex treatment planning is required, for example combined periodontal and endodontal problems.
- Those with predisposing medical conditions, for example organ transplant patients.
- Those at risk of complications from dental treatment.
Where do I find an endodontist?
You can find a board-certified endodontist at the American Board of Endodontics directory at http://www.aae.org/
How much will an endodontist charge?
Root canal costs are going to vary depending on which tooth is affected, how many root canals are needed and who your endodontist is. However, you can expect the costs of a general practitioner to range between $400 and $600 for a front tooth and between $500 and $900 a tooth for the back teeth or molars. An endodontist, specializing in tooth root problems, may charge up to 50 percent more.
What happens at an appointment with an endodontist?
History taking
The aim of history taking is to gain an insight into the nature and character of the symptoms of the tooth. The history, freely given by you, is a crucial part of the information gathering process. The endodontist will also be able to clarify if there are contributory or etiological factors in your personal, dental or medical history. The history may also reveal potential complications or potential modifications to treatment planning, for example if you have a phobia of dentists or have had a very bad experience at a previous visit.
Examination of the face
The face is checked for:
- Asymmetry
- Swelling or lymph nodes enlargement
- Pain in the chewing muscles
- Painful swellings or inflammation of the lymph nodes
- Pus discharge on the face
- Temporo-mandibular joint (TMJ) pain/clicking
Examination of tooth involved
A detailed examination of the area(s) of discomfort is carried out.
- Palpation test – finger pressure is applied to the gums on either side of the area of complaint
- Percussion test – the tooth concerned is gently tapped with the end of a mirror handle
- Mobility test – tooth movement is checked and graded according to severity. Excessive mobility may be due to loss of attachment as a result from periodontal disease or inflamed periodontal ligament from pulpitis or occlusal trauma
- Periodontal probing – a detailed periodontal examination is carried out
- Occlusal examination – any signs of excess occlusal loading or trauma, fracture, parafunction and muscle pain
- Assessment of teeth – any signs of tooth decay and whether the tooth is restorable is noted
- Discolored teeth – the shade of discoloration, uniformity and extent is checked
Special investigations
The final stage in the assessment of the teeth is the use of special investigations, the commonest of which are vitality testing and radiographic examination.
Vitality testing
The aim of vitality testing is to attempt to assess the health of the pulp. Â The tests assess crudely the responsiveness of the nerve supply.
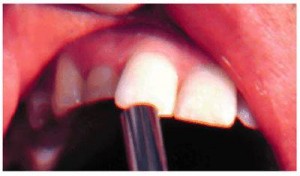
Electric pulp testing
This test involves the use of a battery-operated device to assess pulp vitality. The aim of test is to make a local electrical circuit between the soft tissues in the mouth and the tooth to be investigated.
To be continued in Part 2