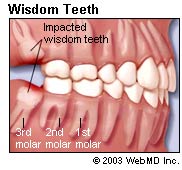
 Wisdom teeth removal are frequently done for wisdom tooth tend to have not enough room to erupt in the jaws, being the last tooth to develop and emerge from the mouth (normally between 18 to 24 years of age), which can cause them to be impacted. If the path of eruption of the tooth is blocked by another tooth or bone which therefore prevents it from assuming a normal position in the mouth, it is called an impacted tooth. Â
Wisdom teeth removal are frequently done for wisdom tooth tend to have not enough room to erupt in the jaws, being the last tooth to develop and emerge from the mouth (normally between 18 to 24 years of age), which can cause them to be impacted. If the path of eruption of the tooth is blocked by another tooth or bone which therefore prevents it from assuming a normal position in the mouth, it is called an impacted tooth. Â
However, not all wisdom teeth need to be removed. Surgical removal of wisdom tooth in absence of any disease or wisdom tooth pain is not usually indicated. However it should be monitored from time to time by clinical examination and radiographs. Decisions about surgery vary widely. Wisdom teeth, impacted, can lead to many complications including pericoronitis and tooth decay.
When to have wisdom teeth extraction
- Recurrent pericoronitis
- Unrestorable tooth decay in the wisdom tooth or its neighbor that cannot be restored
- To facilitate placement of orthodontic appliance or prosthesis
- In presence of pus or severe pain
- Resorption of the tooth or adjacent teeth
- Fracture of wisdom tooth
- Related to a cyst or tumor
- Tooth/teeth preventing jaw reconstruction surgery
- Satisfactory tooth for use as donor for transplantation
General Vs. Local Anesthesia
Surgical removal of wisdom tooth can be done under local anesthesia or general anesthesia. The decision to use either anesthesia depends on the condition of the wisdom tooth and the judgment of the operating dental surgeon.
General anesthesia
General anesthesia is an induced state of unconsciousness or complete loss of protective reflexes, including the lost of ability to continually maintain breathing on your own as well as the ability to respond purposefully to physical stimulation or verbal command.
Indications for general anesthesia
- Medically compromised patients
- Allergy to local anesthesia
- Uncooperative patient with no expectation of behavioral improvement
- Patients with need of a comprehensive dental treatment, for example in a situation where two impacted wisdom teeth need to be removed or where surgery may be technically more difficult.
Contraindications for general anesthesia
Individuals having the following medical conditions are generally not advised to use general anesthesia:
- Upper respiratory tract infection
- Middle ear infection
- Chronic obstructive pulmonary disease
Pros of general anesthesia
- Patient unconscious
- Patient cooperation not absolutely essential
- May be the only method for extremely difficult or mentally handicapped patient that cannot always be managed
- Amnesia during procedure always present
- Less dental visits if more than one wisdom tooth is indicated for removal
Cons of general anesthesia
- Pre-anesthetic medications and fasting required
- Protective reflexes depressed
- Advanced training required (dentist must not act as an anesthetist)
- Detainment in recovery area or hospital stay is necessary
- Special equipment necessary
- More expensive
Local anesthesia
Local anesthesia has been defined as a loss of sensation in a specific area of the body without inducing a loss of consciousness.
Indications for local anesthesia
- Most one-sided wisdom tooth impaction not presenting particular difficulty.
Contraindications to local anesthesia
- Immaturity
- Mental or physical handicap
- Acute infection
- Individuals which need prolonged treatment sessions
- Allergy
- Medical conditions, for example liver disease
- Bleeding disorders
Pros of local anesthesia
- Less expensive
- Only certain part of the body is anaesthetized
- Â Pre-anesthetic medications and fasting not required
- Detainment in recovery area or hospital stay is not required
- Special equipment not necessary
Cons of local anesthesia
- More dental visits required if more than one wisdom tooth is indicated for removal
- Amnesia during procedure not present
The most significant complication encountered is overdosage. Other complications that may happen include:
- Failure to adequately anesthetize the area.
- Pain felt during injection.
- Temporary paralysis of the facial nerve on the face.
- Trismus (prolonged spasm of the jaw muscles in which the normal opening of mouth is restricted).
- Hematoma (blood clot formation within the face tissues)
- Intravascular injection (injection of anesthetic solution into blood vessels).
- Biting of lower lip or tongue.
- Oral ulcers.
- Long-lasting anesthesia.
- Drug interactions.
- Psychogenic reactions or hallucination depending on the type of anesthesia used.
- Allergic reactions to local anesthetic solutions, infections and needle breakage are rare.
What to do after wisdom tooth removal and during wisdom teeth recovery
- Bite on a gauze pack as instructed by your dental surgeon for 15 to 20 minutes.
- Take rest and avoid physical activities.
- If pain is felt, take painkillers as prescribed by your dental surgeon.
- Avoid eating if the numbness of the anesthesia persists.
- Avoid warm food as it can result in bleeding. In addition, soft diet is advised.
- An ice pack may help reduce inflammation and swelling.
- Avoid brushing the involved area on the day of surgery. After 24 hours rinse mouth with warm saline solution to keep wound clean. Resume normal oral hygiene routine two days after surgery.
- Avoid biting the lips or cheek when anesthesia persists.


