Common behaviors seen in children and adults with jaw deficits and subsequent speech and feeding disorders are that of maladaptive oral habits. Such habits include jaw clenching and teeth grinding (bruxism), excessive mouthing of objects, thumb and finger sucking, tongue sucking, lip chewing, nail biting, and extended bottle and pacifier use. These habits, when excessive or are continued past appropriate developmental necessity, can lead to poor dental health, be socially stigmatizing, and inhibit the development of speech clarity.
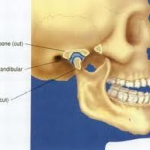 The temporomandibular joint (TMJ) is located near your ears where the mandible and maxilla meet. The joint is used to open and close the jaw with controlled, graded movement. Oral habits such as those listed above are each activities that stimulate the TMJ. The TMJ is the most active joint in the body and a sight of sensory organization and stimulation. As a result, oral habits emerge as a way to achieve desired stimulation. In adults, such input is more commonly achieved through gum chewing, ice crunching, nail biting, and bruxism.
The temporomandibular joint (TMJ) is located near your ears where the mandible and maxilla meet. The joint is used to open and close the jaw with controlled, graded movement. Oral habits such as those listed above are each activities that stimulate the TMJ. The TMJ is the most active joint in the body and a sight of sensory organization and stimulation. As a result, oral habits emerge as a way to achieve desired stimulation. In adults, such input is more commonly achieved through gum chewing, ice crunching, nail biting, and bruxism.
While the jaw is the foundation of oral-motor and speech movements, it is also the site of the TMJ and associated with maladaptive oral habits that affect many children and adults with speech and feeding disorders. Speechlanguage pathologists (SLP’s) are often faced with questions about oral habits and issues such as drooling and mouthing when treating children with speech and language delays and disorders. Common suggestions for remediation of undesirable oral habits are behavioral. This article; however, will suggest physiological reasons why these habits may occur and offer solutions to replace and extinguish undesirable oral habits.
Three common reasons oral habits may occur include: environmental/external stress, dental misalignment (malocclusions) and physical tension located in the TMJ, and weakness due to instability and underuse of the oral musculature. Environmental or external stress is normal and processed differently in each person. Some feel tension in their shoulders, stomachs, or get frequent headaches; while others may exhibit tension in the oral musculature and TMJ. The maladaptive behaviors listed above can be signs of associated stress or tension. While this can be a normal and adaptive behavior promoting stability, it can also become excessive in those who have associated misuse or lack of use of the jaw and TMJ.
In the second population, the cause of maladaptive oral habits is related to the dental structures. When the upper and lower teeth do not meet functionally there may be a tendency to stimulate the jaw and dentition to improve alignment of the jaw and TMJ and to add sensory stimulation. Orthodontia is the prescribed treatment for malocclusions.
The final population may be the most interesting to SLPs who specialize in the diagnosis and treatment of children and adults with speech and oral-motor deficits. These individuals may also exhibit oral habits to stimulate the TMJ and to organize and stabilize the body, but there is an additional reason why they seem to need more stimulation.
These individuals may evidence low tone and reduced strength in the muscles of the jaw as a result of lack of use of the oral musculature or have difficulty with appropriate movements due to hypotonicity. Prolonged thumb or finger-sucking, continued reliance on bottle-feeding, and refusal to give up a pacifier may be additional behaviors noted in this population.
As speech-language pathologists, our primary goals will be
1) to satisfy the need for stimulation to the TMJ and
2) to increase jaw stability. As stability increases, sensory awareness increases. Therefore, as the muscles of the jaw are used more appropriately, the need to engage in oral habits will decrease. Over a period of time the habit can be eliminated.
There are five important sequential steps that should be acknowledged when attempting to extinguish a habit. First, determine why the individual is demonstrating the observed habit. Stimulation to the TMJ creates calmness and body awareness. Requiring the child to stop the behavior or preventing him/her from engaging in the behaviors may eliminate the behavior temporarily, but it does not address the need for stimulation and the persistence of the habit.
 The second step is to identify why the habit should be eliminated. Does it impact negatively on health, nutritional intake, speech production or dentition? If so, it will be necessary to collect information to explain and validate your recommendation to the family, teachers, or other support team members who will be essential in helping you eliminate the habit.
The second step is to identify why the habit should be eliminated. Does it impact negatively on health, nutritional intake, speech production or dentition? If so, it will be necessary to collect information to explain and validate your recommendation to the family, teachers, or other support team members who will be essential in helping you eliminate the habit.
The third step is to empathize with the client and begin a program plan. Perhaps the only time the individual is content is when he/she is involved in the oral habit. A pacifier is called a pacifier for obvious reasons; the action of horizontal suckling calms the individual. Before you begin therapy, develop a program plan that will supply alternative and adequate sensory stimulation to the TMJ and oral structures. Beginning a program plan should utilize therapy techniques that satisfy the need for TMJ stimulation, do not impact negatively on speech production, and are socially acceptable. A combination of:
a) sensory input with vibration,
b) feeding intervention strategies and
c) oral-motor activities have been the most effective means of improving jaw stability, thereby eliminating the reliance on oral habits for calming. Listed here are some of the feeding and oral-motor techniques available:
1) Chewing:
a) chewing solids on the back molars,
b) chewing on a variety of therapy tools: firm licorice, ARK Probes, ARK Grabbers, Z-Vibes, Chewy Tubes, and
2) oral-motor activities: Gum Chewing Hierarchy (teaches children to chew and not to swallow the gum), Gum Chewing Program, Graduated Bite Blocks, and Jaw Exercisers.
 Once therapy goals have been identified, the forth step is to arrange a conference with the child’s family, teachers or other support team members. In that meeting the therapist can present:
Once therapy goals have been identified, the forth step is to arrange a conference with the child’s family, teachers or other support team members. In that meeting the therapist can present:
a) the reasons why the individual may be relying on the habit,
b) the reasons why the habit should be eliminated and
c) therapy strategies to replace the desired stimuli.
In addition, it will be important to listen to any caregiver concerns and to affirm the habit is not going to be eliminated today. It is going to take time to replace and finally eliminate the behavior(s).
The fifth and final step is to replace the behaviors. Once the program plan is initiated and the child is receiving adequate stimulation to the TMJ, the habit can be extinguished. Remember, we do not want to eliminate the habit until a substitute is in place. For example, if a child is still drinking from a bottle at age three and is unable to receive adequate liquid nutrition from a cup or straw, then eliminating the bottle-feeding habit would compromise the child’s nutritional integrity. It is essential to teach the child to drink therapeutically from a cup or straw before any attempt to eliminate the bottle should be made.
In conclusion, remember: techniques to eliminate the undesirable oral habit should be introduced when a program plan, which will outline the replacement behaviors, is established and when family and caregiver support is in place.

Yes, you are right children teeth needs lot of care. So parents should aware of children dental problem.
Thanks for sharing informative post.