Continued from Part 1
HIV disease
HIV disease (symptomatic HIV infection) appears as the CD4 count progressively declines over a long incubation period, which may extend over 5 to 15 years or more. Then the person may develop:
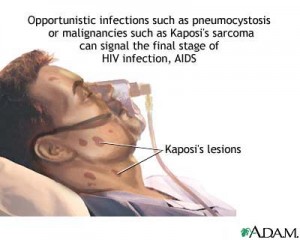
- Infections: the most important infections are pneumonia, candidiasis, herpesviruses and parasites. Opportunistic infections are common and resistant to treatment. Tuberculosis is increasing in HIV-infected persons in whom it may invoke mycobacteria resistant to a range of anti-tubercular drugs. Pneumocystis carinii pneumonia (PCP) is a lung infection seen in up to 80% of infected persons and is the immediate cause of death in up to 20% of individuals dying with AIDS.
- Tumors: the main tumors appear to be virally related and include Kaposi sarcoma associated HHV-8, lymphomas associated with EBV, and cervical and anal cancers associated with HPV.
-
Anorexia, diarrhea, wasting, premature aging and autoimmune phenomena particularly thrombocytopenic purpura.
-
Sometimes neuropsychiatric disease: there may be dementia complex, with personality changes, ataxia and convulsions, and other cerebral syndromes.
AIDS
AIDS is the most severe manifestations of HIV infection. Persons living with AIDS often have weight loss, diarrhea, oropharnygeal candidiasis, infections of the lungs, brain, eyes and other organs, Kaposi sarcoma and lymphoma, and AIDS dementia complex.
Prognosis of HIV / AIDS
The prognosis of HIV / AIDS has almost invariably been poor and death virtually inevitable, although there are rare patients who show remarkable genetic resistance. Anti-retrovirals have been developed that can significantly slow the progression of HIV disease.
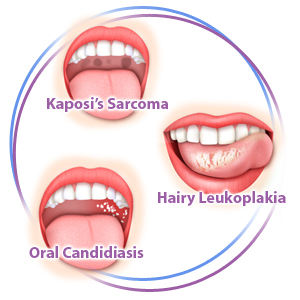
Oral symptoms of HIV infection
Oral features of HIV / AIDS reflect the T-cell immune defect and are, thus, mainly the consequence of fungal or viral infections.
The most common are candidiasis (candidosis) and hairy leukoplakia. Necrotizing gingivitis, accelerated periodontitis, Kaposi sarcoma, lymphomas, salivary gland disease, ulcers of various infective causes and other lesions may be seen.
Oral lesions may indicate HIV infection that is previously undiagnosed, be used in staging and therapy decisions, or cause the individual pain or esthetic problems.
These oral diseases have a number of common features, namely that generally they are:
-
not absolutely specific for HIV / AIDS, but are more a manifestation of the immune defect; thus similar lesions can be seen in other immune defects,
-
generally more likely to manifest as the CD4 cell count falls to low levels,
-
more likely to be seen where the oral hygiene is poor,
-
more likely where there is also malnutrition,
-
more likely if the person smokes tobacco,
-
often controlled, at least temporarily, by anti-retroviral treatment.
Classification of oral lesions in HIV disease
Group I: lesions strongly associated with HIV infection
-
Candidiasis: erythematous, hyperplastic, thrush (pseudomembranous)
-
Hairy leukoplakia (EBV)
-
HIV gingivitis
-
Necrotizing ulcerative gingivitis
-
HIV periodontitis
-
Kaposi sarcoma
-
Non-Hodgkin’s lymphoma
Group II: lesions less commonly associated with HIV infection
-
Atypical ulceration (oropharnygeal)
-
Idiopathic thrombocytopenic purpura
-
Salivary gland diseases: dry mouth, unilateral or bilateral swelling of major salivary glands
-
Viral infections (other than EBV): cytomegalovirus, herpes simplex virus, human papilloma virus (warty-like lesions), varicella-zoster virus – herpes zoster and varicella
Group III: lesions possibly associated with HIV infection
A miscellany of rare disease
Diagnosis of HIV infections
Considerable compassion is required in the diagnosis of such as a catastrophic infection, since it impacts on virtually all aspects of the person’s life as well as that of their family and others, eventually resulting in unpleasant, painful and incapacitating illnesses and their treatment. There must always be appropriate counseling:
-
HIV infection at the very early stage may manifest no detectable antibody production and thus the test for serum HIV antibodies (serotesting) is negative – but this is then a false-negative result. At this stage only sophisticated tests for HIV RNA will detect the virus.
-
HIV serum antibodies usually become detectable by 6 weeks.
- The enzyme-linked immunosorbent assay (ELISA) for HIV p24 antibodies is the main serological HIV test used, but mus be repeated and may need to be confirmed by a Western blot test. False test reactions are known, but rare.
Management of HIV disease
Few, if any, patients have spontaneous remission and thus treatment is almost invariably indicated, although in rare cases the disease progresses very slowly and may only at a very late stage manifest with serious complications.
Since AIDS was first recognized about 20 years ago, remarkable progress has been made in improving the quality and duration of life of HIV-infected persons. Early intervention with anti-retroviral drugs is usually beneficial. Treatment with a combination of these drugs is termed highly active antiretroviral therapy (HAART). There is some controversy as to the increase in heart disease and heart attacks, at which point therapy should be introduced and as to the importance of prophylaxis of infections. Post-exposure prophylaxis (PEP) is by short-term antiretroviral treatment to lessen the likelihood of HIV infection after potential exposure. Vaccines against HIV are still very much in their infancy.