Signs and symptoms
Signs vary widely based on which type of EDS the patient has. In each case, however, the signs are ultimately due to faulty or reduced amounts of collagen. EDS most typically affects the joints, skin, and blood vessels. Following is a list of major signs and symptoms.
Musculoskeletal:
- Hyper-flexible joints (It is possible to be very flexible or have “double joints”, however, this is not the same as EDS.)
- Unstable joints that are prone to: sprain, dislocation, subluxation and hyperextension
- Early onset of advanced osteoarthritis
- Chronic degenerative joint disease
- Swan neck deformity of the fingers
- Muscle fatigue that increases with use
- Weak muscle tone (hypotonia) in infancy, which can delay the development of gross motor skills such as sitting,     standing, and walking
- Osteopenia (low bone density)
- Stretchy ligaments and tendons
- Tearing of tendons or muscles
- Deformities of the spine, such as: Scoliosis (curvature of the spine), Kyphosis (a thoracic hump), Tethered spinal cord syndrome, Occipitoatlantoaxial hypermobility
- Myalgia (muscle pain) and arthralgia (joint pain)
Skin:
- Stretchy skin with a velvety texture
- Fragile skin that tears easily
- Easy bruising, which can be severe
- Abnormal wound healing and scar formation, leading to widened atrophic scars
- Redundant skin folds
- Molluscoid pseudotumors, especially on pressure points
- Subcutaneous spheroids
- Fatty growths on forearms or shins
- Angioplasia
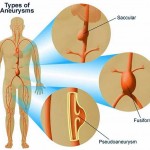
- Fragile blood vessels with tendency towards aneurysm (even abdominal aortic aneurysm)
- Unpredictable rupture of arteries
- Valvular heart disease (such as mitral valve prolapse, which creates an increased risk for infective endocarditis during surgery, as well as possibly progressing to a life-threatening degree of severity of the prognosis of mitral valve prolapse)
- Orthostatic intolerance, likely due to an excessive distension of veins that causes blood to pool in the lower limbs in response to an upright posture
- Dilation and/or rupture of ascending aorta
- Cystic medial necrosis
- Varicose veins
- Vascular skin conditions: Raynaud’s phenomenon, Livedo reticularis
Other Complications:
- High and narrow palate, resulting in dental crowding
- Early-onset periodontitis
- Nearsightedness, which may be extreme
- Blue sclera
- Retinal detachment
- Flat feet
- Digestive disorders: (gastritis, gastroesophageal reflux disease,irritable bowel syndrome, diverticulitis, gastroparesis (partial paralysis of the stomach))
- Hiatial hernia
- Anal prolapse
- Dysautonomia
- Vulnerability to chest and sinus infections
- Collapsed lung (pneumothorax)
- Intestinal/uterine fragility or spontaneous rupture
- Nerve compression disorders (carpal tunnel syndrome, acroparesthesia, neuropathy)
- Insensitivity to local anesthetics.
- Arnold-Chiari malformation (brain disorder)
- Cranial instability
- Migraines
- Problems with proprioception including dysmetria
- Talipes equinovarus (club foot),  especially in the Vascular type
- Platelet aggregation failure (platelets do not clump together properly)
- Bleeding diathesis
- Petechiae
- Cerebrospinal fluid leak (rent in the meningeal tissues: dura, arachnoid)
- Temporomandibular joint syndrome
- Surgical complications and intraoperative problems due to tissue fragility
- Pregnancy complications: increased pain, mild to moderate peripartum bleeding, cervical insufficienty, uterine tearing , or premature rupture of membranes.
Because it is often undiagnosed or misdiagnosed in childhood, some instances of Ehlers–Danlos syndrome have been mischaracterized as child abuse. The pain associated with this condition is a serious complication.
Genetics
 Mutations in the following can cause Ehlers–Danlos syndrome:
Mutations in the following can cause Ehlers–Danlos syndrome:
- Fibrous proteins: COL1A1, COL1A2, COL3A1, COL5A1, COL5A2, and TNXB
- Enzymes: ADAMTS2, PLOD1, B4GALT7
Mutations in these genes usually alter the structure, production, or processing of collagen or proteins that interact with collagen. Collagen provides structure and strength to connective tissue throughout the body. A defect in collagen can weaken connective tissue in the skin, bones, blood vessels, and organs, resulting in the features of the disorder.
Inheritance patterns depend on the type of Ehlers–Danlos syndrome. Most forms of the condition are inherited in an autosomal dominant pattern, which means only one of the two copies of the gene in question must be altered to cause the disorder. The minority are inherited in an autosomal recessive pattern, which means both copies of the gene must be altered for a person to be affected by the condition. It can also be an individual (de novo or “sporadic”) mutation. Please refer to the summary for each type of Ehlers–Danlos syndrome for a discussion of its inheritance pattern.
Diagnosis
A diagnosis can be made by an evaluation of medical history and clinical observation. The Beighton scale is widely used to assess the degree of joint hypermobility. Both DNA and biochemical studies can be used to help identify affected individuals. In some cases, a skin biopsy has been found to be useful in confirming a diagnosis. Unfortunately, these tests are not sensitive enough to identify all individuals with EDS. If there are multiple affected individuals in a family, it may be possible to perform prenatal diagnosis using a DNA information technique known as a linkage study.