Palatal Implants
 One of the limitations of using implants for orthodontic anchorage is having adequate bone. Conventional root-form implants require adequate thickness of bone for placement, thus limiting their use to edentulous areas. Several authors have reported the midsagittal area of the hard palate as a suitable site for a short implant.
One of the limitations of using implants for orthodontic anchorage is having adequate bone. Conventional root-form implants require adequate thickness of bone for placement, thus limiting their use to edentulous areas. Several authors have reported the midsagittal area of the hard palate as a suitable site for a short implant.
Block and Hoffman devised a system that allowed placement of osseointegrated implant anchors in the midpalatal region of the maxilla. In 1989 they designed the Onplant system (Nobel Biocare, Göteborg, Sweden). The device in this system is a thin (2 mm thick and 10 mm in diameter) titanium alloy disk that has a textured side that opposes bone and is coated with a 75 μm layer of hydroxyapatite.
The side facing soft tissue is smooth titanium alloy with a threaded hole in the center into which abutments are placed. Original designs of the disks included a sharp (90°) angle at the periphery, but this design was later altered to prevent adverse soft tissue reactions at this margin.
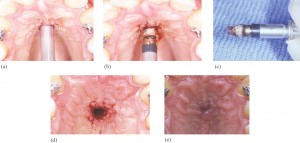
Onplants are placed subperiosteally on the posterior aspect of the hard palate. A “tunneling†procedure is used to place these anchors. A fullthickness mucoperiosteal incision is made on the anterior aspect of the hard palate, and tunnels are reflected posteriorly. These tunnels allow the onplant to be placed away from the incision, thus reducing the potential for soft tissue reactions that prevent osseointegration. A healing screw is placed, and 10 to 12 weeks are allowed for integration. After this healing period, a small amount of tissue is removed over the healing screw, which is replaced by an abutment.
In addition to requiring less bone depth for placement compared with endosseous implants, onplants can be loaded after a shorter healing period. The onplant system cuts this healing period approximately in half. Despite these advantages, one area of concern with this system is removal of the onplant.
Like Block and Hoffman, Straumann has devised an implant system that can be placed in areas of decreased bone thickness. In 1996 Wehrbein and colleagues described this system in a pilot study. The Straumann Orthosystem incorporates screw-type endosseous implants that can be placed in the palate and subjected to orthodontic force without migration or loss of osseointegration. In addition to the median palate, the Orthosystem implant can be placed in retromolar positions owing to its design. The self-tapping Orthosystem implant itself has a diameter of 3.3 mm and is available in 4.0 and 6.0 mm lengths. A 4.0 mm diameter implant is also available for use when drilling errors have occurred.
According to Wehrbein and colleagues, the advantages of the Orthosystem are that it can be placed in areas that conventional implants cannot, soft tissue irritation is minimal, and anchorage is stable owing to sound osseointegration.
The disadvantages are that the placement process requires a surgeon, loading is not typically done immediately, and removal of the device often requires the use of a trephine owing to the extent of osseointegration.
Miniscrews
An alternative approach to achieving anchorage is the use of titanium miniscrews. These devices are very small and can be placed in areas where other implantable devices cannot. For example, some miniscrews are so small that they can actually be placed in bone between the roots of individual teeth. The screws themselves are similar or identical to those used for osteotomy fixation following orthognathic surgery. These mini-screws are unique because unlike restorative endosseous implants they do not require osseointegration.
Instead, these devices rely on mechanical retention to maintain rigidity, which also makes their removal relatively simple and noninvasive.
They may be loaded immediately, but biomechanical factors must be taken into consideration owing to the increased chance of loosening associated with the lack of integration and torquing or rotational forces that may occur under loading. Kanomi published one of the preliminary reports of this technique in which he referred to the devices as mini-implants.
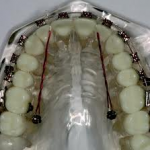
Although he referred to the devices by a different name, his results were essentially similar to those of other case reports on the use of miniscrews, such as the one published by Costa and colleagues. Their article is a case report in which the authors observed 14 patients with 16 screws. The titanium screws that they used were manufactured by a company called Cizeta (Rome, Italy) and had a diameter of 2 mm and a length of 9 mm. The placement technique involved inserting the screws under local anesthesia directly through mucosa without a mucoperiosteal flap. The screws were placed in several different locations depending on the desired treatment and available bone. They were reported to be useful in both the maxilla and the mandible, specifically, on the inferior surface of the anterior nasal spine, midpalatal suture, infrazygomatic crest of the maxilla, retromolar area of the mandible, and mandibular symphysis and within edentulous areas of the alveolar process. After taking into account what tooth movements were desired, the location was decided upon, and the screws were placed with specific angulations to accommodate existing anatomy and deliver forces in the desired directions. Prior to insertion of the screws, a 1.5 mm diameter hole was drilled into the bone with a slow-speed handpiece using irrigation.
The miniscrews were inserted by hand with a screwdriver. To apply the desired force, the heads of the screws were joined to the dental arch or tooth with a wire. In cases involving one-dimensional force, the head of the screw was placed so that mucosa would cover it and the attached wire would emerge from the mucosa. In cases that involved the use of multidimensional forces, the heads of the screws were kept above the mucosa so that edgewise wires could be inserted into the specially designed head of the screw.