Bullae may present on any oral or oropharyngeal surface, but typically arise in the buccal, palatal and gingival regions. Occasional patients have lesions restricted completely to the gingiva. Skin lesions are similar except that the more heavily keratinized epidermis allows blisters to remain intact much longer. Most patients have circulating autoantibodies which can be detected by indirect immunofluorescence using serum from other affected individuals. Titers are directly proportionate to the severity of the disease.
A special subset of patients demonstrates internal malignancy in addition to mucosal and skin erosions and bullae. Called paraneoplastic pemphigus, its oral manifestations may resemble erythema multiforme or bullous lichen planus and may be extremely severe and resistant to treatment. The associated autoantibodies are different from those of routine pemphigus vulgaris, and can be demonstrated by indirect immunofluorescence using rat bladder transitional epithelium as the substrate. Pemphigus vulgaris only shows positive indirect immunofluorescence on stratified squamous epithelium, such as monkey esophagus. Neoplasms most often associated with this form of pemphigus include lymphoma, leukemia, sarcoma and thymus tumors. Waldenstrom’s macroglobulinemia and Castleman’s disease have also been reported as associated.
Rare variants of pemphigus may affect the oral mucosa. Pemphigus vegetans presents with much smaller blisters than pemphigus vulgaris. The blisters are often filled with pus and coalesce to impart an appearance of vegetative growth. The vermilion border of the lips is especially prone to involvement. The oral disease most likely to clinically mimic this form of pemphigus is pyostomatitis vegetans, a rare oral manifestation of inflammatory bowel disease, particularly ulcerative colitis and Crohn’s disease. Oral lesions in this disease are characterized by yellow, partially ulcerated pustules arranged in serpentine strands or “snail tracks” on an erythematous background. Minimal discomfort is felt and the oral lesions may precede intestinal involvement.
Pemphigus foliaceus may affect perioral and other facial skin. The least severe form of pemphigus, pemphigus erythematosus, presents on the face and scalp with scaly dermal erythema reminiscent of seborrheic dermatitis. There may be a “butterfly” erythema of the nose and midface, mimicking lupus erythematosus. Oral and pharyngeal lesions are in these subtypes extremely rare.
Pathology and Differential Diagnosis
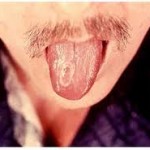
The blistering or cleavage in this disease occurs above the basal layer of the epithelium, typically leaving a layer of basal cells with rounded tops, reminiscent of tombstones. The intact bulla is filled with serum and occasional sloughed, rounded, keratinocytes resembling fried eggs, with large, hyperchromatic nuclei and a rim of eosinophilic cytoplasm . The latter acantholytic cells, called Tzanck cells, are best seen in the smear sample of a fresh blister (Tzanck test). They are strongly suggestive of pemphigus vulgaris but may also be encountered in Darier’s disease and in regenerating thermally- or chemically-damaged epithelium. The suprabasal bulla frequently contains chronic and acute inflammatory cells, including eosinophils. The presence of eosinophils in oral vesiculoulcerative lesions is somewhat unique, but may also occur in pemphigoid, epidermolysis bullosa acquisita, eosinophilic granuloma, parasitic infection and traumatic eosinophilic ulcer.
When the bulla has ruptured, the associated ulcer bed slowly becomes covered with fibrinoid necrotic debris, with neovascularity and mixed inflammatory cells in the underlying stroma. The epithelium at the edge of a fresh ulcer will show intraepithelial cleavage.
Direct immunofluorescence of perilesional mucosa shows a lacy or chicken-wire pattern of deposits around individual spinous cells of the epithelium. IgG is almost always the deposited immunoglobulin, but IgM and IgA are seen in almost half of all cases. Some authorities have suggested direct immunofluorescence of cytologic smears as a reliable and noninvasive method of diagnostic confirmation. Direct immunofluorescence of paraneoplastic pemphigus mucosa demonstrates both intercellular and basement membrane IgG and complement deposits.
Differentiation from other oral and pharyngeal bullous diseases is easily made, because most of them produce subepithelial blisters (pemphigoid, epidermolysis bullosa, bullous lichen planus, linear IgA disease), but small lesions may be mistaken for intraepithelial viral vesicles and any lesion may be confused with the oral keratinized blisters of Darier’s disease. Clinical history or the presence of syncytial multinucleated epithelial cells will usually lead to a diagnosis of infection by a dermatotrophic virus capable of damaging oral mucosa, e.g. herpes simplex, herpes zoster and Coxsackie viruses, while the presence of excessive surface keratinization and cor ronds within intact bullae will help to differentiated Darier’s disease.
Finally, it is important to remember that mucosal lesions of erythema multiforme may demonstrate either intraepithelial or subepithelial blistering, or both. This unique allergic response, however, typically occurs in much younger patients, has a much more abrupt onset and has a limited duration, making it relatively easy to distinguish it from pemphigus.
Treatment and Prognosis
Systemic corticosteroid therapy is effective in reducing or eliminating the clinical manifestations of pemphigus vulgaris, although doses of prednisone may have to be as high as 400 mg. daily for patients with severe involvement. Topical corticosteroids can be used as an adjunct therapy if the bullae are confined to oral mucosa. Oral or intravenous administration of cyclophosphamide, azathioprine, cyclosporine and methotrexate may have enough beneficial effect to allow reduced dosages of corticosteroids. Even with immunosuppressive therapy, however, almost 10% of patients will die from their disease, either from electrolyte loss, wound infection or treatment complications. Patients with paraneoplastic pemphigus may have to forgo treatment of their vesiculobullous disease until the underlying neoplasm is controlled, although supportive therapy can be instituted.