FAILURES IN FIXED PARTIAL DENTURE
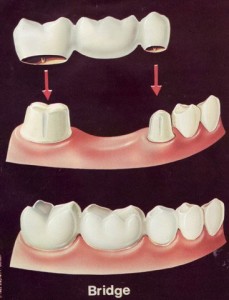
A bridge is a custom-made device anchored to neighboring natural teeth, which replaces one or more missing teeth. When a lost tooth is replaced with bridgework, the teeth on either side of the missing one are prepared as crowns to hold the bridge in place. Bridges, sometimes referred to as a fixed partial denture, look natural and literally bridge the gap where one or more teeth may have been. Fixed bridges appear and function similar to natural teeth.
INTRODUCTION:
DENTAL RESTORATIONS ,NO MATTER HOW CAREFULLY PLACED, MAY REQUIRE MODIFICATION OR
REPLACEMENT. THE ORIGINAL EVALUATION AND TREATMENT SHOULD HAVE ENSURED GOOD ABUTMENT SELECTION , CROWN PREPARATION WITH ADEQUATE MARGIN PLACEMENT, PONTIC DESIGN AND CORRECT OCCLUSION. NO GUARANTEE CAN BE GIVEN CONCERNING THE LONGEVITY OF ANY PROSTHESIS . PATIENTS SOMETIMES CAN PRESENT WITH ONE OF A NUMBER OF MAJOR PROBLEMS AFTER CROWNS OR FIXED PARTIAL DENTURES HAVE BEEN CEMENTED.
CAUSES OF FAILURE
- Caries
- Pulp degeneration
- Periodontal breakdown
- Occlusal problems
- Tooth perforation
- Temperomandibular disorders
- Mechanical failures:
- Loss of retention
- Connector failure
- Occlusal failure
- Cementation failure
- Tooth fracture/ root fracture
- Porcelain fracture
- Maintenance failures
- Esthetic failures
- Facing failures
Caries:
- One of the most common biologic failures.
- Usually perceived by the patient as
- Â Pain or sensitivity to hot ,cold or sweet foods & liquids.
- Dysgeusia
- Halitosis
- Loose restorations
- Fractured teeth
- Discolored teeth
Small lesions :
- Gold foil – filling material of choice for restoring marginal caries.
- Amalgam – best alterative to gold foil filling because ofits ability to produce long term marginal seal.
- Composite – indicated for restoration of caries in esthetic zone.
- Glass ionomer cement.
- Proximal lesions :
- Removal of prosthesis is required to obtain access to caries.
- If the lesion is small, the tooth preparation can be extended to eliminate the caries and a new prosthesis can be fabricated.
- When the lesion is large, an amalgam restoration is often required.
- An extensive lesion may require endodontic treatment when pulp has been encroached.
- A grossly destroyed teeth by caries that cannot be restored must be extracted.
- Schwartz et al (1970) & Randow et al (1986) both reported caries to be the most frequent cause of failure of existing restorations (36% & 18.3%).
- Glantz et al .in 1993 reported that of 77 bridges reviewed at 15yrs , 32.5% required removal. Further reported in 1993 that the incidence of caries was not related to the age of the patient , rather , to the time that the bridge had functioned .
Pulp degeneration:
- This is usually perceived by the patient as:
- pain – either spontaneous or related to hot or cold or sweet stimuli.
- pain which is accentuated by lying down or exercise
Causes :
- Extensive preparation
- Excess heat generation during preparation
- Indication for endodontic treatment
- Post insertion pulpal sensitivity on abutment teeth that doesn’t subside with timeà intense painà periapical pathology detected radiographically
Management:
- Access preparation – a hole is drilled in the prosthesis through which the biomechanical preparation (BMP) is completed.
- The access cavity is restored with
- Gold foil
- Amalgam
- Cast metal inlay
- If the retainer come loose during access opening or if the porcelain fractures, then remaking of the prosthesis may be necessary.
- A post and core restoration should be considered if little sound tooth structure is remaining.
- Survival of endodontically treated , post-restored teeth depends on a multitude of factors , all of which are practically impossible to include in a randomized , controlled clinical study.
Following conclusions were derived:
- Fracture of the tooth was the most common type of failure among the failed post-retained restorations followed by loosening of the post & fracture .
- Tapered posts more often displayed fracture of the tooth and less often fracture of the post.
- Fracture of the post was more common among male patients than among female patients.
- Periodontal breakdown:
- This is usually perceived by the patient as:
- Looseness of teeth or bridgework
- Drifting teeth
- Bleeding tissues
- Changes in color of the gums
- Bad breath
- Bad taste
- Pain
- Abscess formation
- Poor aesthetics
- Periodontal disease can produce extensive bone loss , which in course of time results in the loss of abutment teeth and attached prosthesis.
- Aspects of the prosthesis that interfere with effective plaqueremoval include:
- Poor marginal adaptation
- Overcontouring of the axial surfaces of the retainers
- Excessively large connectors that restrict cervical embrasure space
- A pontic that contacts too large an area on the edentulous ridge.
- A prosthesis with rough surfaces which promote plaque accumulation.
Management :
- Plaque accumulation à Prophylaxis, removal of local factor
- Tissue hyperplasia à Gingivoplasty
- Devitalized & severe bone lossà Endodontic procedure/ bicuspidization hemisection of teeth.
- Less severe breakdown can be treated without fear of loss of teeth, with small surgery which may produce an unacceptablerelationship between prothesis & the soft tissue.
Occlusal problems:
- Patients may be uncomfortable with their new occlusions.
- Some patients tolerate gross occlusal discrepancies without complaining , whereas others are intolerant to discrepancies
- in the range of 10-15 microns.
- Occlusal discomfort is perceived by the patient as:
- General discomfort with the “biteâ€
- Sore teeth
- Loose teeth or bridges
- Sensitive teeth
- “Tired†or “sore†muscles
- Interfering centric and eccentric occlusal contacts can cause:
- Excessive tooth mobility
- Irreversible pulpal damage
Management :
- When detected early occlusal adjustment should be done to eliminate these interferences without permanent damage.
- Occasionally, a combination of excessive mobility and reduced bone support require extraction of abutment teeth.
- Irreversible pulpal damage requires endodontic treatment.
- Change in vertical dimension:
- VD may be decreased as a result of severe attrition or increased as a result of poor restorative planning.
- Porcelain occlusal surfaces in short clinical crowns-vd increases
- Following symptoms may be perceived by the patient:
- Altered facial appearance
- Dribbling of saliva à loss of VD can precipitate “angular chelitisâ€
- Extreme changes in VD can convert an asymptomatic
- internal derrangement into a symptomatic one.à alteration in muscle activity can cause “myalgiaâ€.
- Extreme increase in VD reduces ability of tongue to create a seal during swallowing
- Compensating movement of the larynx during swallowing
- Muscle strain & symptoms such as “sore throat†or “tired tongueâ€
- Teeth can become sensitive either due to loss of occlusal tissue or due to trauma to the teeth from the increased VD.
- Clenching of teeth because of premature contact.
- Loss of posterior vertical dimension à lower anterior teeth occluding more heavily with the palatal surface of the upper anterior teeth causing drifting or failure of anterior restorations.
- Decrease in the VD can result in occluding of the lower incisors with the palatal soft tissues giving rise to soreness & possible periodontal complications.
- Decrease or increase in VD
- Difficulty in mastication
- Gross increase in the VD
- Speech problems particularly with sibilants.
Tooth perforation:
- Improperly located pinholes or pins used in conjunction with pin-retained restorations may perforate the tooth laterally.
- Management : depends on the location of the perforation.
- Occlusal to periodontal ligament
- Extend the preparation to cover the defect.
- Extends into periodontal ligament
- Perform periodontal surgery
- Smoothening of the projecting pin
- Place a restoration into perforated area
- Furcation region
- Surgically inaccessible
- Severe periodontal problems may ultimately
- lead to extraction of the tooth.
- Pulp chamber
- Endodontic treatment
- Subpontic inflamation:
- Perceived by the patient as :
- Pain
- Swelling
- Bad breath
- Bad taste
- Bleeding gums
- Poor esthetics