1. What are the best methods for detecting early and advanced dental caries (validity and feasibility of traditional methods; validity and feasibility of emerging methods)?
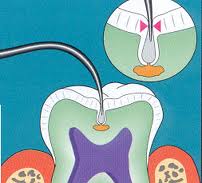
Observations and studies during the past two decades have indicated that diagnostic and treatment paradigms may differ significantly for large, cavitated lesions versus early, small lesions and demineralized areas on tooth surfaces. The essential anatomic-pathophysiologic problem is that the carious lesion occurs within a small, highly mineralized structure following penetration through the structure’s surface in a manner which may be difficult to detect using current methods. Additionally, carious lesions occur in a variety of anatomic locations, often adjacent to existing restorations, and have unique aspects of configuration and rate of spread. These differences make it unlikely that any one diagnostic modality will have adequate sensitivity and specificity of detection for all sites. The application of multiple diagnostic tests to the individual patient increases the overall efficacy of caries diagnosis. Existing diagnostic modalities require stronger validation, and new modalities with appropriate sensitivities and specificities for different caries sites, caries severities, and degrees of caries activity are needed.
A systematic review, based on predefined criteria, concluded that studies of reliability and reproducibility of existing diagnostic modalities, which included visual-tactile, radiographic, and electrical conductance examinations, were not strong. The most significant problems with these studies were weak study designs; variability of examiner calibration; differences in criteria for lesions; lack of standards for histological validation; lack of adequate numbers of studies on several modalities and types of caries; and the sensitivity and specificity of caries detection. Also, given the acceptance criteria of the systematic review, which excluded all studies without histologic confirmation, the results regarding the validities of the examined modalities were ambiguous.
A number of studies excluded by the systematic review were also addressed. The use of sharp explorers in the detection of primary occlusal caries appears to add little diagnostic information to other modalities and may be detrimental. Studies employing receiver operating characteristic (ROC) analyses have shown radiology to have acceptable diagnostic efficacy in detecting larger cavitated lesions in numerous in vitro and in vivo studies. There was agreement that the literature is weak in the areas of diagnosis of caries on root surfaces and adjacent to existing restorations. The problems of assessing the microbiological load of demineralized dentin adjacent to or beneath existing restorations, and differentiating between residual and secondary caries, are substantial and important. Digitally acquired and postprocessed images have great potential in the detection of noncavitated caries and in the diagnosis of secondary caries. Promising new diagnostic techniques are emerging, including fiber-optic transillumination and light and laser fluorescence. These new modalities and developing digital imaging systems require robust laboratory and clinical evaluation.
Existing diagnostic modalities appear to have satisfactory sensitivity and specificity in diagnosing substantial, cavitated, dental caries; specifically radiographic methods are essential in diagnosing interproximal carious lesions. However, these modalities do not appear to have sufficient sensitivity or specificity to efficaciously diagnose noncavitating caries, root surface caries, or secondary caries. There is currently no diagnostic modality which can differentiate between microbiologically active caries and demineralized dentin without caries activity beneath a restoration. This is a critical weakness in view of the significant percentage of restorations inserted to replace existing restorations. The need for the identification and clinical staging of the presence, activity, and severity of dental caries is of paramount importance in the deployment of treatment strategies that employ increasingly important nonsurgical modalities, such as fluoride, antimicrobials, sealants, and no treatment. Some diagnostic modalities are currently in various stages of development and testing; these modalities will need to be evaluated, using rigorously controlled clinical trials. Such studies will promote true staging of carious lesions, based on highly sensitive and specific diagnoses, followed by appropriate, linked, treatment-planning decision algorithms.
2. What are the best indicators for an increased risk of dental caries?
Recent decades have seen a remarkable decline in dental caries in the United States. The level of caries incidence, however, is not evenly distributed in the population. Overall, 20 percent of the population bears at least 60 percent of the caries burden while fewer that 5 percent of adults are caries-free. Thus, effective dentistry requires early identification of children at high risk for extensive caries so that they may receive early and intense preventive intervention, as well as those at low risk so as to reduce unnecessary care and associated expenditures. Caries incidence changes in adulthood and in geriatric populations, and risk and risk indicators may differ due to changes in host and environmental characteristics. Accurate caries prognosis throughout the life span, however, can support an appropriate, individualized level of care for each patient and a more effective use of health care resources for the individual and for the population. In addition, as dentistry moves towards earlier detection of lesions and a more preventive rather than restorative orientation, good risk assessment will be essential for improving the predictive values of new screening and diagnostic methods by preselecting at-risk subpopulations.