Continued from Part 1
Diagnosis and treatment planning for bone defects and furcation involvement
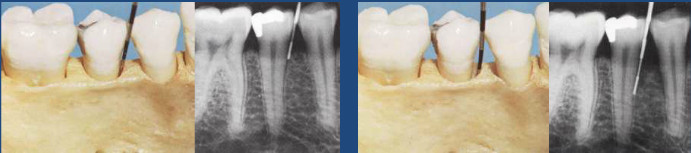 Careful radiographic or x-ray examination is done but it may not reveal the presence of a bone defect or its precise morphology.
Careful radiographic or x-ray examination is done but it may not reveal the presence of a bone defect or its precise morphology.
Direct examination of bone morphology:
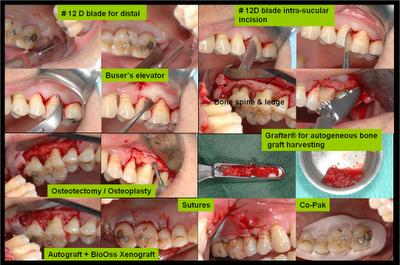
- Lift a full thickness mucoperiosteal flap
- Granulations are curetted and root surfaces planed clean
- Alveolar crest examined, morphology of bone defect can be defined
- Mode of treatment decided
Three basic treatment options are available:
- Bone reshaping so that after healing and remodeling the resultant alveolar architecture will allow effective oral hygiene measures to be carried out
- To obtain some bony fill-in with or without bone grafts
- To obtain new connective tissue attachment with guided tissue regeneration
Bone reshaping
Osteoplasty is a procedure that involves shaping bone that is not directly attached to the tooth. Indicated for thickened and uneven alveolar margins, marginal gutters, interdental craters, and two wall bony defect.
Ostectomy is a procedure involving the removal of bone that is directly involved in tooth support. Bone may be removed by chisels or rotating instruments.
Bone swaging is a bone reshaping technique whereby a piece of bone is incompletely detached from its base (by a chisel) and swung into a neighboring bone defect with some of its blood supply maintained.
Periodontal tissue regeneration
The term ‘reattachment’ is used to describe the reunion of root and connective tissue separated by incision or surgery.
‘New attachment’ describes the union of connective tissue with a previously pathogenically altered root surface.
The tooth supporting cells with regenerative potential in the periodontal wound are:
- junctional epithelial cells,
- gingival connective tissue,
- bone cells,
- periodontal ligament cells
Outcome of periodontal therapy
- Epithelial cells – long junctional epithelium
- Gingival connective tissue cells – fibers parallel to tooth surface, resorption of root surface
- Bone cells – ankylosis (fusion of root to the jaw bone)
- Periodontal ligament cells – new cementum and periodontal ligament, bone
The ideal outcome of periodontal therapy is to have periodontal ligament cells as they have the capacity to develop new attachment if epithelium and gingival connective tissues are excluded from the wound during healing.
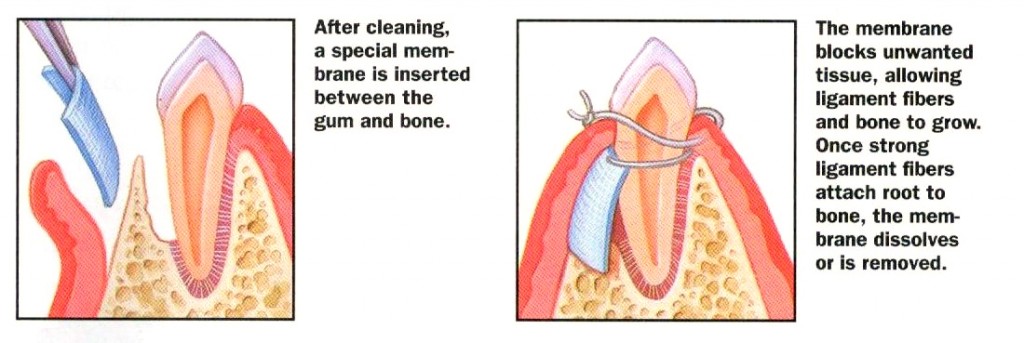
Guided tissue regeneration
The principle of the guided tissue regeneration technique:
- Exclusion of junctional epithelium and gingival connective tissue from the wound by a membrane
- Allow time for periodontal ligament cells to migrate coronally (towards the crown) and differentiate into functional cells for the three periodontal tissues – bone, cementum, and periodontal ligament
Guided tissue regeneration membrane
| Biodegradable membrane | Non degradable membrane |
| Resorbed by body after a few weeks | Not resorbed by body |
| Need not be removed | Need to be removed after 4 to 6 weeks |
| For example polylactic acid | For example expanded polytetrafluoroethylene membrane |
Methods of regeneration of periodontal tissues
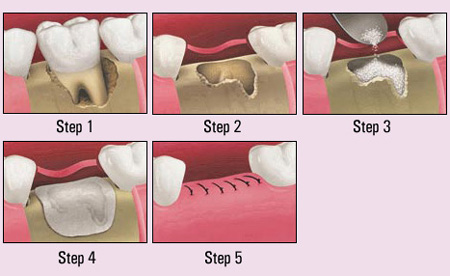
Curettage for bony fill-in is the complete removal of inflammatory tissues from bony defects and careful root planning often results in some bony fill-in. bony fill-in is produced by bone cells called osteoblasts from the surrounding marrow spaces in the jaw bone.
Factors that can prevent bone fill
- Choosing the wrong type of defect
- Failure to curette away all inflamed connective tissues
- Failure to clean root surface completely
- Failure to close flaps completely over the bone socket
- Infection and disintegration of the blood clot
- Excessive tooth mobility
Bone grafts
Bone fill-in by simple curettage is unpredictable. Bone grafts are used induce or promote regrowth and regeneration of bone. A number of graft materials can be used to fill in the bony defect.
Types of bone grafts
- Bone autograft
- Bone allograft
- Bone xenografts
- Synthetic bone substitutes
Bone autograft
Bone autografts are bone taken from the same individual and are obtained from the iliac crest or oral cavity. Cancellous bone and marrow are obtained from various sites in the mouth such as the tuberosity, extraction sockets, and edentulous ridges.
Bone allograft
Bone allografts are bone taken from an individual of the same species. Â Freeze dried bone allograft are used to treat periodontal bony defects. There are two types of bone allograft:
- Freeze-dried undemineralized bone allograft (FDBA),
- Freeze-dried demineralized bone allograft (FDDBA)
The freeze drying permits storage within a vacuum for an indefinite shelf life and also markedly reduced the antigenicity (body rejection) of graft
Bone xenografts
Bone xenografts are bone taken from a different species such as cows and pigs.
- Bovine inorganic cancellous bone from cows
- Porcine non antigenic collagen produced from healthy pigs
Synthetic bone substitutes
These materials are preferred as antigenic potential is absent and risks of infection are less. Synthetic bone substitutes include porous and non-porous hydroxyapatite, beta tricalcium ohosphate, HTR polymer, and bio-active glasses and ceramics.