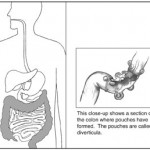
Diverticulitis is a common digestive disease particularly found in the large intestine. Diverticulitis develops from diverticulosis, which involves the formation of pouches (diverticula) on the outside of the colon. Diverticulitis results if one of these diverticula becomes inflamed.
Signs and symptoms
 Patients often present with the classic triad of left lower quadrant pain, fever, and leukocytosis (an elevation of the white cell count in blood tests). Patients may also complain of nausea or diarrhea; others may be constipated.
Patients often present with the classic triad of left lower quadrant pain, fever, and leukocytosis (an elevation of the white cell count in blood tests). Patients may also complain of nausea or diarrhea; others may be constipated.
Less commonly, an individual with diverticulitis may present with right-sided abdominal pain. This may be due to the less prevalent right-sided diverticula or a very redundant sigmoid colon.
Diverticulitis
The most common symptom of diverticulitis is abdominal pain. The most common sign is tenderness around the left side of the lower abdomen. If infection is the cause, then nausea, vomiting, fever, cramping, and constipation may occur as well. The severity of symptoms depends on the extent of the infection and complications. Diverticulitis may worsen throughout the first day, as it starts as small pains and/or diarrhea, and may slowly turn into vomiting and sharp pains.
Diverticulosis
Most people with diverticulosis do not have any discomfort or symptoms; however, symptoms may include mild cramps, bloating, and constipation. Other diseases such as inflammatory bowel disease (IBD) and stomach ulcers cause similar problems, so these symptoms do not always mean a person has diverticulosis.
Causes
 The development of colonic diverticulum is thought to be a result of raised intraluminal colonic pressures. The sigmoid colon (Section 4) has the smallest diameter of any portion of the colon, and therefore the portion which would be expected to have the highest intraluminal pressure. The claim that a lack of dietary fiber, particularly non-soluble fiber (also known in older parlance as “roughage”) predisposes individuals to diverticular disease was long accepted within the medical literature. However, the first study to specifically test the theory has found that “A high-fiber diet and increased frequency of bowel movements are associated with greater, rather than lower, prevalence of diverticulosis.”
The development of colonic diverticulum is thought to be a result of raised intraluminal colonic pressures. The sigmoid colon (Section 4) has the smallest diameter of any portion of the colon, and therefore the portion which would be expected to have the highest intraluminal pressure. The claim that a lack of dietary fiber, particularly non-soluble fiber (also known in older parlance as “roughage”) predisposes individuals to diverticular disease was long accepted within the medical literature. However, the first study to specifically test the theory has found that “A high-fiber diet and increased frequency of bowel movements are associated with greater, rather than lower, prevalence of diverticulosis.”
Diet
Foods such as seeds, nuts, and corn were, in the past, thought by many health care professionals to possibly aggravate diverticulitis. However, recent studies have found no evidence that suggests the avoidance of nuts and seeds prevents the progression of diverticulosis to an acute case of diverticulitis. Not only has this research shown that they do not appear to be aggravating the diverticulitis, but it appears that a higher intake of nuts and corn could in fact help to avoid diverticulitis in male adults.
Diagnosis
People with the above symptoms are commonly studied with a computed tomography, or CT scan. The CT scan is very accurate (98%) in diagnosing diverticulitis. In order to extract the most information possible about the patient’s condition, thin section (5mm) transverse images are obtained through the entire abdomen and pelvis after the patient has been administered oral and intravascular contrast. Images reveal localized thickening and hyperemia (increased blood flow) involving a segment of the colon wall, with inflammatory changes extending into the fatty tissues surrounding the colon. The diagnosis of acute diverticulitis is made confidently when the involved segment contains diverticulae. CT may also identify patients with more complicated diverticulitis, such as those with an associated abscess. It may even allow for radiologically guided drainage of an associated abscess, sparing a patient from immediate surgical intervention.
Other studies, such as barium enema and colonoscopy are contraindicated in the acute phase of diverticulitis due to the risk of perforation.
Differential diagnosis
 The differential diagnosis includes colon cancer, inflammatory bowel disease, ischemic colitis, and irritable bowel syndrome, as well as a number of urological and gynecological processes. Some patients report bleeding from the rectum.
The differential diagnosis includes colon cancer, inflammatory bowel disease, ischemic colitis, and irritable bowel syndrome, as well as a number of urological and gynecological processes. Some patients report bleeding from the rectum.
Treatment
Most cases of simple, uncomplicated diverticulitis respond to conservative therapy with bowel rest and antibiotics. The evidence for antibiotics however in mild cases is poor. However, recurring acute attacks or complications, such as peritonitis, abscess, or fistula may require surgery, either immediately or on an elective basis.
People may be placed on a low residue diet. This low-fiber diet gives the colon adequate time to heal without needing to be overworked. Later, patients are placed on a high-fiber diet.
Surgery
Diverticulitis surgery may be elective or may be a medical emergency. Whether the elective surgery should be performed is decided by external factors such as the stage of the disease, the age of the patient and his or her general medical condition, as well as the severity and frequency of attacks or if the symptoms persisted after a first acute episode. In most cases, the decision to perform elective surgery is taken when the risks of the surgery are smaller than the ones resulted from the complication of the condition. Elective surgery may be performed at least six weeks after recovery from acute diverticulitis.